خواص دارویی و گیاهی

A total of 149 drugs are known to interact with Nexium (esomeprazole).
Show all medications in the database that may interact with Nexium (esomeprazole).
Type in a drug name to check for interactions with Nexium (esomeprazole).
View interaction reports for Nexium (esomeprazole) and the medicines listed below.
There is 1 alcohol/food interaction with Nexium (esomeprazole)
nexium 40 mg drug interactions
There are 4 disease interactions with Nexium (esomeprazole) which include:
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer
Some mixtures of medications can lead to serious and even fatal consequences.
Here are 9 ways to stay safe
Latest: Heartburn Drugs Might Bring Allergy Woes
omeprazole, amoxicillin, pantoprazole, ranitidine, metronidazole, famotidine, Protonix, Zantac, Prilosec, Dexilant
Nexium reviews
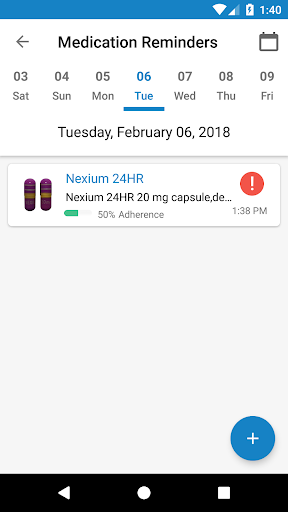
The easiest way to lookup drug information, identify pills, check interactions and set up your own personal medication records. Available for Android and iOS devices.
Subscribe to Drugs.com newsletters for the latest medication news, alerts, new drug approvals and more.
Drugs.com provides accurate and independent information on more than 24,000 prescription drugs, over-the-counter medicines and natural products. This material is provided for educational purposes only and is not intended for medical advice, diagnosis or treatment. Data sources include IBM Watson Micromedex (updated 1 Aug 2019), Cerner Multum™ (updated 1 Aug 2019), Wolters Kluwer™ (updated 31 July 2019) and others.
Third Party Advertising
We comply with the HONcode standard for trustworthy health information – verify here
Copyright © 2000-2019 Drugs.com. All rights reserved.
A total of 149 drugs are known to interact with esomeprazole.
Show all medications in the database that may interact with esomeprazole.
Type in a drug name to check for interactions with esomeprazole.
View interaction reports for esomeprazole and the medicines listed below.
There is 1 alcohol/food interaction with esomeprazole
nexium 40 mg drug interactions
There are 4 disease interactions with esomeprazole which include:
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer
Some mixtures of medications can lead to serious and even fatal consequences.
Here are 9 ways to stay safe
Latest: Heartburn Drugs Might Bring Allergy Woes
omeprazole, amoxicillin, pantoprazole, ranitidine, metronidazole, famotidine, Nexium, Protonix, Zantac, Prilosec
Esomeprazole reviews
The easiest way to lookup drug information, identify pills, check interactions and set up your own personal medication records. Available for Android and iOS devices.
Subscribe to Drugs.com newsletters for the latest medication news, alerts, new drug approvals and more.
Drugs.com provides accurate and independent information on more than 24,000 prescription drugs, over-the-counter medicines and natural products. This material is provided for educational purposes only and is not intended for medical advice, diagnosis or treatment. Data sources include IBM Watson Micromedex (updated 1 Aug 2019), Cerner Multum™ (updated 1 Aug 2019), Wolters Kluwer™ (updated 31 July 2019) and others.
Third Party Advertising
We comply with the HONcode standard for trustworthy health information – verify here
Copyright © 2000-2019 Drugs.com. All rights reserved.
Department of Pharmacology, S.C.S. College of Pharmacy, Harapanahalli – 583 131, Karnataka, India
1College of Clinical Pharmacy, King Faisal University, Alahsa – 31982, Kingdom of Saudi Arabia
Department of Pharmacology, S.C.S. College of Pharmacy, Harapanahalli – 583 131, Karnataka, India
Department of Pharmacology, S.C.S. College of Pharmacy, Harapanahalli – 583 131, Karnataka, India
Department of Pharmacology, S.C.S. College of Pharmacy, Harapanahalli – 583 131, Karnataka, India
nexium 40 mg drug interactions
Drug–drug interaction between esomeprazole at therapeutic and higher doses and sulfonylureas was studied. Sulfonylureas (tolbutamide 40 mg/kg and glibenclamide 40 µg/kg) were administered and the time to onset of hypoglycemia, the duration of the hypoglycemia, and the peak hypoglycemia were determined. Esomeprazole (1.8 mg/kg, 3.6 mg/kg, and 30 mg/kg) was administered for 8 days and its influence on sulfonylurea-induced hypoglycemia was studied. Therapeutic doses of esomeprazole, i.e., 1.8 mg/kg and 3.6 mg/kg dose did not influence the hypoglycemia induced by sulfonylureas. However, a higher dose, i.e., 30 mg/kg, did significantly enhance the duration of hypoglycemia and the peak hypolgycemia. Esomeprazole (30 mg/kg) by itself did not reduce the blood glucose levels; therefore, a pharmacodynamic type of drug interaction can be ruled out. Similarly, a pharmacokinetic type of drug interaction may be ruled out at therapeutic doses. The CYP isoenzyme system involved in the metabolism of sulfonylureas are not very sensitive to esomeprazole and the dose and frequency of administration of sulfonylurea need not be readjusted when they are used concomitantly with esomeprazole (at therapeutic doses).
Drug–drug interactions may occur when more than one drug is administered in a patient to treat a single ailment or multiple ailments. These concomitantly used drugs may either cause pharmacodynamic or pharmacokinetic types of interactions. The net result of both the types of interactions is the alteration in the therapeutic effect of either or both the drugs. There are several diseases that require treatment for the lifetime, e.g., diabetes and hypertension. Patients with such diseases will often need to be administered drugs for treatment of other co-existing diseases, either for a short period or lifelong. There is then a possibility of occurrence of interactions between drugs, resulting in either reduced or enhanced effects of any of the drugs. Therefore, monitoring and readjustment of the dose/s is often necessary to optimize treatment. In the present study, two diseases (diabetes and gastric ulcers) that may co-exist and require chronic treatment were considered and the occurrence of interaction between the concurrently used drugs was assessed
Diabetes mellitus is a disease characterized by elevated blood glucose levels. It requires treatment for prolonged periods, usually lifelong. Diabetic patients may also have other diseases, e.g., peptic ulcers, infectious diseases, etc. In such situations, treatment for the different ailments will have to be given simultaneously. Peptic ulcer is one such disorder that requires treatment for a prolonged period. There are several patients who suffer from both diabetes and peptic ulcers. In such patients, H2-receptor blockers or proton pump inhibitors are administered concomitantly with sulfonylureas or insulin preparations. There are reports that H2-receptor blockers such as ranitidine inhibit the metabolism of sulfonylureas and enhance their bioavailability.[1,2] Similarly, there are reports that chronic usage of omeprazole increases the peak concentration and apparent elimination half-life of phenytoin in healthy male volunteers.[3] CZP2C9 is the enzyme responsible for the metabolism of phenytoin and sulfonylureas. Therefore it is hypothesized that esomeprazole may influence the metabolism of study drugs. In addition, there is a report that omeprazole increased the duration of hypoglycemia and peak hypoglycemia induced by sulfonylureas in healthy albino rabbits.[4] One report has been published showing that proton pump inhibitors like lansoprazole induce the cytochrome-P450 enzyme system.[5] Lansoprazole at two dose levels – 30 mg/kg and 60 mg/kg for 7 days – significantly enhanced the duration of hypoglycemia induced by tolbutamide and the peak hypoglycemia slightly; the time to onset of hypoglycemia was not altered significantly. Similarly, pretreatment with lansoprazole has been shown to enhance the peak hypoglycemia and the duration of hypoglycemia induced by glibenclamide in healthy rabbits.[6] Pretreatment with pantoprazole, 10 mg/kg for 7 days, increased the peak hypoglycemia and the duration of action of glipizide in healthy rabbits and rats as well as in diabetic rats.[7] However, there are no such reports regarding interactions between esomeprazole and antidiabetic agents. Hence, the present study planned to assess the interaction between esomeprazole and oral antidiabetic agents such as tolbutamide and glibenclamide.
The esomeprazole used in this study was from Micro Labs Ltd., Bangalore; the tolbutamide from Albert David Ltd., Bombay; and the glibenclamide from Aventis Pharma Ltd., Goa.
Albino rats of either sex, weighing 150–250 g, were procured from Sri. Venkateshwara Enterprises, Bangalore, and were stored under standard husbandry conditions. They were used for the study after a 7-day acclimatisation period. Permission for the usage of animals and approval of the experimental protocols for the study was obtained from the institutional animal ethics committee prior to the experimentation. The Registration No. for institutional animal house is 157/1999/CPCSEA.
Albino rats of either sex (150–250 g), maintained under standard conditions, were randomly distributed into 6 groups of 6 animals each. The experiment was conducted in two phases. In the first phase, after fasting for 18 hours all the animals of groups 1, 2, and 3 were administered tolbutamide (40 mg/kg) and groups 4, 5, and 6 were given glibenclamide (40 µg/kg) orally. Zero-hour blood samples were collected for estimation of fasting blood glucose levels. Blood samples were collected at 0.5, 1, 2, 3, 4, 6, 8, 12, 18, 24, 30, 36, 42, and 48 hours from the tail vein of all the rats after drug treatment. Blood glucose levels were estimated.[8] In the second phase, after 1 day of the respective sulfonylurea treatment, the animals of groups 1 and 4 received esomeprazole 1.8 mg/kg, groups 2 and 5 received esomeprazole 3.6 mg/kg, and groups 3 and 6 received esomeprazole 30 mg/kg for a period of 8 days. During this period the animals had free access to food and water supplied ad libitum. On the 7th day, the rats were fasted for 18 hours, with water supplied ad libitum. On the 8th day, esomeprazole was administered and the zero-hour blood sample was collected from all the animals of all the groups. The animals of groups 1, 2, and 3 were administered tolbutamide (40 mg/kg) and groups 4, 5, and 6 were given glibenclamide (40 µg/kg) orally. Blood samples were collected at the above-mentioned prefixed time intervals and blood glucose levels were estimated.
The data is presented as mean±standard error of the mean. Analysis was by using Student’s ‘t’ test. P≤0.05 is considered as statistically significant.
Esomeprazole 30 mg/kg per se did not alter the blood glucose levels [Figure 1]. Tolbutamide 40 mg/kg and glibenclamide 40 µg/kg induced a peak hypoglycemia of 68.47±2.01 mg% and 70.17±2.09 mg%, respectively. The time to onset of hypoglycemia (i.e., the time taken to achieve at least 20% reduction in blood glucose levels) by both the drugs was about 1 hour, and the duration of hypoglycemia (i.e., the duration for which at least 20% reduction in blood glucose level maintained) was 40 h. However, esomeprazole at doses of 1.8 mg/kg and 3.8 mg/kg did not influence the hypoglycemia induced by tolbutamide and glibenclamide. The results are shown in Tables Tables11 and and2.2. The pilot studies showed no influence of pretreatment with esomeprazole (up to 20 mg/kg) on the hypoglycemia induced by oral tolbutamide and glibenclamide. Therefore, we tried to assess the influence of more than eight times the therapeutic dose of esomeprazole (i.e., 30 mg/kg) on hypoglycemia induced by sulfonylureas. Tolbutamide- and glibenclamide-induced hypoglycemia was enhanced significantly by pretreatment with esomeprazole at the dose of 30 mg/kg; Pretreatment with esomeprazole enhanced the tolbutamide induced peak hypoglycemia from 59.11±3.78 mg% to 64.53±1.05 mg% and glibenclamide induced peak hypoglycemia from 64.97±1.42 mg% to 72.05±4.93, mg% respectively. Similarly, the duration of hypoglycemia was also enhanced significantly. The results are compiled in.
Blood glucose level with esomeprazole (30 mg/kg) in healthy rat
Percentage blood glucose reduction with tolbutamide in healthy albino rats before and after esomeprazole
Percentage blood glucose reduction with glibenclamide in healthy albino rats before and after esomeprazole
Esomoprazole at 30 mg/kg dose did not by itself reduce the blood glucose level, indicating that any interaction with antidiabetic drugs in this study is not of the pharmacodynamic type. In the present study, therapeutic doses of esomeprazole did not influence any of the parameters of the hypoglycemia induced by sulfonylureas. However, at 8 times the therapeutic dose, esomeprazole enhanced the duration of hypoglycemia as well as the peak level of hypoglycemia induced by sulfonylureas. The literature reports reveal that sulfonylureas are metabolized mainly by CYP2C9 and CYP3A.[9] At the dose of 30 mg/kg esomeprazole probably inhibits these isoenzymes. Since it requires eight times the therapeutic doses of esomeprazole to inhibit the CYP isoenzymes that are responsible for metabolism of sulfonylureas, these enzymes apparently have low sensitivity/affinity for esomeprazole.
It may be concluded that during concomitant administration of sulfonylureas and esomeprazole at therapeutic doses, drug–drug interaction does not occur. Therefore, the therapeutic dose and the frequency of administration of sulfonylureas need not be adjusted.
The authors are highly indebted to the management of TMAE society and the SCS college of Pharmacy, Harapanahalli, for providing basic facilities and financial assistance.
Source of Support: TMAE society and the SCS college of Pharmacy, Harapanahalli
Conflict of Interest: None declared.
National Center for
Biotechnology Information,
U.S. National Library of Medicine
8600 Rockville Pike, Bethesda
MD, 20894
USA
%PDF-1.7
%
3883 0 obj
>
endobj
3909 0 obj
>/Filter/FlateDecode/ID[]/Index[3883 56]/Info 3882 0 R/Length 120/Prev 523380/Root 3884 0 R/Size 3939/Type/XRef/W[1 3 1]>>stream
hbbd“`b“”KZ)”րH20D5`6,RI`n
Not a Member?
Register Now
Email this page
Send the page “”
to a friend, relative, colleague or yourself.
Separate multiple email address with a comma
We do not record any personal information entered above.
nexium 40 mg drug interactions
Thank you. Your email has been sent.
Proton Pump Inhibitors/PPIs
Rx, OTC
Proton pump inhibitor (PPI); S-isomer of omeprazoleUsed for GERD, NSAID-induced ulcer healing and prevention, erosive esophagitis, H. pylori eradication, upper GI rebleeding prophylaxis after therapeutic endoscopy, and hypersecretory conditions; available OTC for heartburnAvoid concomitant use with clopidogrel; consider using a PPI with less CYP2C19 inhibitory activity
Nexium, Nexium 24HR
Esomeprazole/Esomeprazole Magnesium/Esomeprazole strontium/Nexium/Nexium 24HR Oral Cap DR Pellets: 20mg, 24.65mg, 40mg, 49.3mgEsomeprazole/Esomeprazole Sodium/Nexium Intravenous Inj Pwd F/Sol: 40mgEsomeprazole/Esomeprazole Sodium/Nexium Intravenous Pwd: 20mgNexium Nasogastric Pwd F/Recon: 2.5mg, 5mg, 10mg, 20mg, 40mgNexium Oral Pwd F/Recon: 2.5mg, 5mg, 10mg, 20mg, 40mg
20 mg PO once daily given 60 minutes before first meal of the day for 4 weeks. If symptoms persist, an additional 4 weeks of treatment may be considered. Per treatment guidelines, initiate empiric therapy based on a presumptive diagnosis of GERD in the setting of typical symptoms of heartburn and regurgitation. For patients with partial response to once daily therapy, consider an increase in dose to esomeprazole 20 mg PO twice daily or consider a one-time switch to a different PPI. Refer non-responders for further evaluation. Consider maintenance therapy for patients who continue to have symptoms after PPI discontinuation; the lowest effective dose, including on demand or intermittent therapy should be used with regular assessment of the need for continued PPI therapy. Alternatively, step down maintenance therapy to an H2 blocker is acceptable.
20 mg PO once daily, taken 1 hour before meals for 4 weeks. Alternatively, a dose range of 0.7 to 3.3 mg/kg/day PO is recommended by the American Academy of Pediatrics (AAP). Do not exceed recommended adult doses (20 to 40 mg/day).
10 mg PO once daily, taken 1 hour before meals, for up to 8 weeks. Alternatively, a dose range of 0.7 to 3.3 mg/kg/day PO is recommended by the American Academy of Pediatrics (AAP).
Esomeprazole was not more effective than placebo in a 4-week, placebo-controlled study (data not published). Doses of 0.25 mg/kg/day and 1 mg/kg/day PO were used in a short-term pharmacokinetic study (n = 45). After 1 week of treatment, the 1 mg/kg/day dose provided similar exposure to that seen in adults receiving 20 mg/day PO; this dose also provided the most effective acid suppression. Both doses of esomeprazole were well tolerated. PPIs are not recommended as first-line therapy for symptomatic GERD in otherwise healthy infants (1 to 11 months); non-pharmacologic measures such as diet modification and positioning strategies are preferred. Reserve pharmacologic treatment for use in infants with disease diagnosed by endoscopy (e.g., esophageal erosion).
Safety and efficacy have not been established; esomeprazole was not superior to placebo in 1 small randomized controlled trial. Doses of 0.5 mg/kg/day PO were used for up to 14 days in a randomized, placebo controlled study of premature and term neonates (n = 52, gestational ages 24 to 40 weeks) with symptoms of gastroesophageal reflux disease (GERD). There were no significant differences in the total number of GERD-related signs and symptoms or the total number of reflux episodes in patients receiving esomeprazole compared to those receiving placebo. Patients receiving esomeprazole did have significantly fewer acidic reflux episodes compared to patients receiving placebo. Esomeprazole was well tolerated.
24.65 mg PO once daily given 60 minutes before first meal of the day for 4 weeks. If symptoms persist, an additional 4 weeks of treatment may be considered. Per treatment guidelines, initiate empiric therapy based on a presumptive diagnosis of GERD in the setting of typical symptoms of heartburn and regurgitation. For patients with partial response to once daily therapy, consider an increase in dose to esomeprazole 24.65 mg PO twice daily or consider a one-time switch to a different PPI. Refer non-responders for further evaluation. Consider maintenance therapy for patients who continue to have symptoms after PPI discontinuation; the lowest effective dose, including on demand or intermittent therapy should be used with regular assessment of the need for continued PPI therapy. Alternatively, step down maintenance therapy to an H2 blocker is acceptable.
Initially, 40 mg PO twice daily. Adjust dosage to attain clinical goals. Doses up to 240 mg/day PO have been administered. Patients have been treated for up to 12 months.
Initially, 49.3 mg PO twice daily. Adjust dosage to attain clinical goals. Esomeprazole equivalent doses up to 240 mg/day PO have been administered.
NOTE: Esomeprazole magnesium trihydrate 22.3 mg capsules contain 20 mg of esomeprazole.
20 mg (1 capsule) PO once daily with a full glass of water, an an empty stomach in the morning for 14 days. Full relief may take 1—4 days. If frequent heartburn returns, patients may repeat a 14-day course of treatment every 4 months. Do not exceed 1 capsule/day PO, treatment for 14 days, or repeat courses more frequently than every 4 months, unless directed to do so by a healthcare provider.
40 or 80 mg PO once daily in combination with clarithromycin and either amoxicillin or metronidazole for 14 days.
49.3 or 98.6 mg PO once daily in combination with clarithromycin and either amoxicillin or metronidazole for 14 days.
40 mg PO once daily as part of a combination therapy as a first-line treatment option. Quadruple therapy includes a proton pump inhibitor (PPI) in combination with clarithromycin, amoxicillin, and metronidazole for 10 to 14 days. Hybrid therapy includes amoxicillin plus PPI for 7 days followed by PPI in combination with clarithromycin, amoxicillin, and metronidazole for 7 days. Sequential therapy includes PPI and amoxicillin for 5 to 7 days followed by PPI in combination with clarithromycin and metronidazole for 5 to 7 days.
49.3 mg PO once daily as part of a combination therapy as a first-line treatment option. Quadruple therapy includes a proton pump inhibitor (PPI) in combination with clarithromycin, amoxicillin, and metronidazole for 10 to 14 days. Hybrid therapy includes amoxicillin plus PPI for 7 days followed by PPI in combination with clarithromycin, amoxicillin, and metronidazole for 7 days. Sequential therapy includes PPI and amoxicillin for 5 to 7 days followed by PPI in combination with clarithromycin and metronidazole for 5 to 7 days.
40 mg PO once daily in combination with clarithromycin, amoxicillin, and metronidazole for 10 to 14 days. For patients with a penicillin allergy, a PPI is recommended in combination with clarithromycin and metronidazole for 14 days.
49.3 mg PO once daily in combination with clarithromycin, amoxicillin, and metronidazole for 10 to 14 days. For patients with a penicillin allergy, a PPI is recommended in combination with clarithromycin and metronidazole for 14 days.
40 mg PO twice daily in combination with amoxicillin and metronidazole for 14 days. Triple therapy with standard-dose amoxicillin, metronidazole, and a proton pump inhibitor (PPI) is a first-line treatment option for patients infected with H. pylori strains with known susceptibility to metronidazole and resistance to clarithromycin. Triple therapy with high-dose amoxicillin, metronidazole, and a PPI is a first-line treatment option for patients infected with H. pylori strains with dual resistance to clarithromycin and metronidazole or strains with unknown susceptibility.
30 mg PO twice daily in combination with amoxicillin and metronidazole for 14 days. Triple therapy with standard-dose amoxicillin, metronidazole, and a proton pump inhibitor (PPI) is a first-line treatment option for patients infected with H. pylori strains with known susceptibility to metronidazole and resistance to clarithromycin. Triple therapy with high-dose amoxicillin, metronidazole, and a PPI is a first-line treatment option for patients infected with H. pylori strains with dual resistance to clarithromycin and metronidazole or strains with unknown susceptibility.
20 mg PO twice daily in combination with amoxicillin and metronidazole for 14 days. Triple therapy with standard-dose amoxicillin, metronidazole, and a proton pump inhibitor (PPI) is a first-line treatment option for patients infected with H. pylori strains with known susceptibility to metronidazole and resistance to clarithromycin. Triple therapy with high-dose amoxicillin, metronidazole, and a PPI is a first-line treatment option for patients infected with H. pylori strains with dual resistance to clarithromycin and metronidazole or strains with unknown susceptibility.
40 mg PO twice daily in combination with amoxicillin and clarithromycin for 14 days. Triple therapy with standard-dose amoxicillin, clarithromycin, and a proton pump inhibitor is the first-line treatment option for patients infected with fully susceptible H. pylori strains or strains susceptible to clarithromycin but resistant to metronidazole. In cases of penicillin allergy, use metronidazole in place of amoxicillin for patients infected with fully susceptible strains.
30 mg PO twice daily in combination with amoxicillin and clarithromycin for 14 days. Triple therapy with standard-dose amoxicillin, clarithromycin, and a proton pump inhibitor is the first-line treatment option for patients infected with fully susceptible H. pylori strains or strains susceptible to clarithromycin but resistant to metronidazole. In cases of penicillin allergy, use metronidazole in place of amoxicillin for patients infected with fully susceptible strains.
20 mg PO twice daily in combination with amoxicillin and clarithromycin for 14 days. Triple therapy with standard-dose amoxicillin, clarithromycin, and a proton pump inhibitor is the first-line treatment option for patients infected with fully susceptible H. pylori strains or strains susceptible to clarithromycin but resistant to metronidazole. In cases of penicillin allergy, use metronidazole in place of amoxicillin for patients infected with fully susceptible strains.
40 mg PO twice daily for 10 days. Use in combination with amoxicillin for days 1 through 5, and then clarithromycin and metronidazole for days 6 through 10. Sequential therapy is a first-line treatment option for patients infected with fully susceptible H. pylori strains. Sequential therapy is not recommended if susceptibility testing is unavailable.
30 mg PO twice daily for 10 days. Use in combination with amoxicillin for days 1 through 5, and then clarithromycin and metronidazole for days 6 through 10. Sequential therapy is a first-line treatment option for patients infected with fully susceptible H. pylori strains. Sequential therapy is not recommended if susceptibility testing is unavailable.
20 mg PO twice daily for 10 days. Use in combination with amoxicillin for days 1 through 5, and then clarithromycin and metronidazole for days 6 through 10. Sequential therapy is a first-line treatment option for patients infected with fully susceptible H. pylori strains. Sequential therapy is not recommended if susceptibility testing is unavailable.
40 mg PO twice daily in combination with amoxicillin, metronidazole, and clarithromycin for 14 days. Concomitant quadruple therapy with amoxicillin, metronidazole, clarithromycin, and a proton pump inhibitor is a first-line treatment option for patients infected with H. pylori strains with dual resistance to clarithromycin and metronidazole or strains with unknown susceptibility.
30 mg PO twice daily in combination with amoxicillin, metronidazole, and clarithromycin for 14 days. Concomitant quadruple therapy with amoxicillin, metronidazole, clarithromycin, and a proton pump inhibitor is a first-line treatment option for patients infected with H. pylori strains with dual resistance to clarithromycin and metronidazole or strains with unknown susceptibility.
20 mg PO twice daily in combination with amoxicillin, metronidazole, and clarithromycin for 14 days. Concomitant quadruple therapy with amoxicillin, metronidazole, clarithromycin, and a proton pump inhibitor is a first-line treatment option for patients infected with H. pylori strains with dual resistance to clarithromycin and metronidazole or strains with unknown susceptibility.
40 or 80 mg PO once daily as part of combination therapy as a first-line treatment option. Triple therapy includes esomeprazole 40 mg PO once daily in combination with levofloxacin and amoxicillin for 10 to 14 days. Sequential therapy includes esomeprazole 40 or 80 mg PO once daily in combination with amoxicillin for 5 to 7 days followed by esomeprazole 40 mg PO once daily in combination with levofloxacin and a nitroimidazole for 5 to 7 days. Quadruple therapy includes esomeprazole 80 mg PO once daily in combination with levofloxacin, nitazoxanide, and doxycycline for 7 to 10 days.
nexium 40 mg drug interactions
49.3 or 98.6 mg PO once daily as part of combination therapy as a first-line treatment option. Triple therapy includes esomeprazole 49.3 mg PO once daily in combination with levofloxacin and amoxicillin for 10 to 14 days. Sequential therapy includes esomeprazole 49.3 or 98.6 mg PO once daily in combination with amoxicillin for 5 to 7 days followed by esomeprazole 49.3 mg PO once daily in combination with levofloxacin and a nitroimidazole for 5 to 7 days. Quadruple therapy includes esomeprazole 98.6 mg PO once daily in combination with levofloxacin, nitazoxanide, and doxycycline for 7 to 10 days.
40 mg PO once daily in combination with levofloxacin and amoxicillin for 14 days. Guidelines recommend this triple therapy in patients who have failed clarithromycin-triple or bismuth-quadruple initial therapies and without previous quinolone exposure. Levofloxacin in combination with metronidazole and a PPI for 14 days could be considered for patients with a penicillin allergy who have failed prior bismuth quadruple therapy.
49.3 mg PO once daily in combination with levofloxacin and amoxicillin for 14 days. Guidelines recommend this triple therapy in patients who have failed clarithromycin-triple or bismuth-quadruple initial therapies and without previous quinolone exposure. Levofloxacin in combination with metronidazole and a PPI for 14 days could be considered for patients with a penicillin allergy who have failed prior bismuth quadruple therapy.
40 mg PO once daily in combination with bismuth subcitrate or subsalicylate, metronidazole, and tetracycline for 10 to 14 days is recommended as a first-line treatment option, particularly in patients with any previous macrolide exposure or a penicillin allergy.
49.3 mg PO once daily in combination with bismuth subcitrate or subsalicylate, metronidazole, and tetracycline for 10 to 14 days is recommended as a first-line treatment option, particularly in patients with any previous macrolide exposure or a penicillin allergy.
40 mg PO once daily in combination with rifabutin and amoxicillin for 10 days.
49.3 mg PO once daily in combination with rifabutin and amoxicillin for 10 days.
40 mg PO once daily in combination with bismuth subcitrate or subsalicylate, tetracycline, and metronidazole for 14 days is recommended particularly in patients failing clarithromycin triple therapy. A subsequent repeat course of bismuth quadruple therapy may be considered after failed prior bismuth quadruple therapy.
49.3 mg PO once daily in combination with bismuth subcitrate or subsalicylate, tetracycline, and metronidazole for 14 days is recommended particularly in patients failing clarithromycin triple therapy. A subsequent repeat course of bismuth quadruple therapy may be considered after failed prior bismuth quadruple therapy.
20 to 40 mg PO once daily 60 minutes before first meal of the day for 4 to 8 weeks. For patients who do not heal during the initial treatment course, consider an additional 4 to 8 week course. For maintenance of healing, 20 mg PO once daily; periodically reassess need for continued PPI therapy. Controlled studies do not extend beyond 6 months.
20 mg or 40 mg PO once daily for 4 to 8 weeks. Alternatively, a dosage range of 0.7 to 3.3 mg/kg/day PO is recommended by the American Academy of Pediatrics (AAP). Do not exceed recommended adult doses (20 to 40 mg/day).
0.7 to 3.3 mg/kg/day PO is recommended by the American Academy of Pediatrics (AAP). Do not exceed recommended adult doses (20 to 40 mg/day). The FDA-approved dosage is weight based and administered PO once daily for 8 weeks as follows: 10 mg for weight less than 20 kg; 10 or 20 mg for weight 20 kg or more.
Dosing is weight based and administered PO once daily for up to 6 weeks as follows: 2.5 mg for weight 3 to 5 kg; 5 mg for weight 5.1 to 7.5 kg; and 10 mg for weight 7.6 to 12 kg. Doses greater than 1.33 mg/kg/day PO have not been studied. PPI treatment in infants should be reserved for those with disease diagnosed by endoscopy (e.g., esophageal erosion) and nonpharmacologic measures such as diet modification and positioning strategies are recommended.
Safety and efficacy have not been established; esomeprazole was not superior to placebo in one small randomized controlled trial. Doses of 0.5 mg/kg/day PO were used for up to 14 days in a randomized, placebo controlled study of premature and term neonates (n = 52, gestational ages 24 to 40 weeks) with symptoms of gastroesophageal reflux disease (GERD). There were no significant differences in the total number of GERD-related signs and symptoms or the total number of reflux episodes in patients receiving esomeprazole compared to those receiving placebo. Patients receiving esomeprazole did have significantly fewer acidic reflux episodes compared to patients receiving placebo. Esomeprazole was well tolerated.
24.65 to 49.3 mg PO once daily 60 minutes before first meal of the day for 4 to 8 weeks. For patients who do not heal during the initial treatment course, consider an additional 4 to 8 week course. For maintenance of healing, 24.65 mg PO once daily; periodically reassess need for continued PPI therapy. Controlled studies do not extend beyond 6 months.
20 mg or 40 mg IV infused once daily for up to 10 days. The IV formulation is indicated as an alternative to oral therapy for the short-term treatment of GERD. Switch to oral therapy when feasible.
20 mg IV once daily over 10 to 30 minutes.
10 mg IV once daily over 10 to 30 minutes.
0.5 mg/kg/dose IV once daily infused over 10 to 30 minutes.
Safety and efficacy have not been established; 0.5 mg/kg/dose IV once daily infused over 10 to 30 minutes has been suggested.
80 mg IV bolus infusion over 30 minutes, followed by 8 mg/hour continuous infusion for 71.5 hours after successful endoscopic hemostasis. Per clinical practice guidelines, this regimen may be used in the management of active ulcer bleeding, a non-bleeding visible vessel, or visible adherent clot. Patients with ulcers that have flat pigmented spots or clean bases upon endoscopy can instead receive standard, once daily, oral proton pump inhibitor (PPI) therapy. Pre-endoscopic IV PPI therapy, may be considered in order to downstage the endoscopic lesion. If endoscopic therapy is to be delayed or cannot be performed, IV PPI therapy is recommended to reduce further bleeding. Patients with an underlying etiology for which a PPI may be beneficial (e.g., peptic ulcers, erosions) should be discharged with a prescription for standard, once daily, oral PPI therapy; otherwise, discontinue the PPI before discharge. In clinical trials, after completion of the infusion, patients received oral PPI for 27 days.
20 or 40 mg PO once daily. In clinical trials, the 20 and 40 mg doses showed comparable benefit in providing risk reduction. Roughly 95% of patients remained ulcer free for up to 6 months. Studies did not demonstrate significant reduction in the development of NSAID-associated duodenal ulcer due to the low incidence.
24.65 or 49.3 mg PO once daily. In clinical trials with esomeprazole magnesium, the different doses provided comparable benefits in providing risk reduction. Roughly 95% of patients remained ulcer free for up to 6 months. Studies did not demonstrate significant reduction in the development of NSAID-associated duodenal ulcer due to the low incidence.
20 or 40 mg PO once daily. In a study, the gastric ulcer healing rates at week 8 were 85.7% (95% CI, 79.8% to 91.7%) with esomeprazole 40 mg/day and 84.8% (95% CI, 78.8% to 90.8%) with esomeprazole 20 mg/day; all patients continued to take a nonselective NSAID or a COX-2 inhibitor. In another study of patients with aspirin-related peptic ulcers, gastric ulcer healing rates at week 8 were 82.5% (95% CI, 74.2% to 90.8%) with esomeprazole 40 mg/day and 81.5% (95% CI, 73% to 90%) with esomeprazole 40 mg/day plus aspirin 100 mg/day.
PPI dosing in the range of 20—40 mg PO twice daily 30—60 minutes before meals has been studied; treat for up to 8 weeks and continue until the time of the follow-up endoscopy and biopsy. According to guidelines, a PPI trial is central to the differential diagnosis of EoE. If eosinophilia and symptoms persist on repeat endoscopy and biopsy following a PPI trial, then EoE can be formally diagnosed. If symptoms and eosinophilia resolve, then PPI-REE is diagnosed; PPI-REE patients may or may not have underlying GERD. More than 1/3 of all patients with esophageal eosinophilia on biopsy will respond to a PPI.
Initial doses of 1.1 mg/kg/day PO divided twice daily were used in a small, prospective, open-label study of 12 children aged 2 to 10 years receiving cysteamine therapy. Doses were adjusted during the study based on upper GI symptoms. The mean final dose of esomeprazole was 1.7 mg/kg/day PO (range: 0.7 to 2.75 mg/kg/day PO; Max: 40 mg/day). The authors report a significant decrease in basal gastric acid output and significant improvement in symptom scores.
Dosing is weight based, administered IV once daily, and infused over 10 to 30 minutes as follows: 10 mg IV for weight less than 55 kg; 20 mg IV for weight 55 kg or more.
0.5 mg/kg/dose IV once daily has been suggested.
0.5 mg/kg/dose IV once daily has been suggested.
†Indicates off-label use
20 mg/day PO for heartburn (OTC); 40 mg/day PO is FDA-approved maximum; however, up to 80 mg/day is used off-label for H. pylori eradication; 40 mg/day IV for GERD; 80 mg IV for 1 dose, then 8 mg/hour for upper GI rebleeding prophylaxis after therapeutic endoscopy; up to 240 mg/day PO for Zollinger-Ellison syndrome.
20 mg/day PO for heartburn (OTC); 40 mg/day PO is FDA-approved maximum; however, up to 80 mg/day is used off-label for H. pylori eradication; 40 mg/day IV for GERD; 80 mg IV for 1 dose, then 8 mg/hour for upper GI rebleeding prophylaxis after therapeutic endoscopy; up to 240 mg/day PO for Zollinger-Ellison syndrome.
weight 55 kg or more: 40 mg/day PO is FDA-approved maximum; however, up to 80 mg/day has been used off-label; 20 mg/day IV.weight less than 55 kg: 40 mg/day PO is FDA-approved maximum; however, up to 80 mg/day has been used off-label; 10 mg/day IV.
12 years and weight 55 kg or more: 40 mg/day PO is FDA-approved maximum; however, up to 80 mg/day has been used off-label; 20 mg/day IV.12 years and weight less than 55 kg: 40 mg/day PO is FDA-approved maximum; however, up to 80 mg/day has been used off-label; 10 mg/day IV.1 to 11 years and weight 55 kg or more: 20 mg/day PO and 20 mg/day IV are FDA-approved; however, up to 3.3 mg/kg/day PO (Max: 80 mg/day PO) has been used off-label.1 to 11 years and weight 20 to 54 kg: 20 mg/day PO and 10 mg/day IV are FDA-approved; however, up to 3.3 mg/kg/day PO (Max: 80 mg/day PO) has been used off-label.1 to 11 years and weight less than 20 kg: 10 mg/day PO and 10 mg/day IV are FDA-approved; however, up to 3.3 mg/kg/day PO (Max: 40 mg/day) has been used off-label.
In general for infants, maximum doses are 1.33 mg/kg/day PO and 0.5 mg/kg/day IV.weight 7.6 to 12 kg: 10 mg/day PO; 0.5 mg/kg/day IV.weight 5.1 to 7.5 kg: 5 mg/day PO; 0.5 mg/kg/day IV.weight 3 to 5 kg: 2.5 mg/day PO; 0.5 mg/kg/day IV.
Safety and efficacy have not been established; however, 0.5 mg/kg/day PO/IV has been used off-label.
For most indications, no dosage adjustment is recommended for mild to moderate hepatic impairment. However, in adult patients with severe hepatic insufficiency (Child Pugh Class C), do not exceed 20 mg/day. For upper GI rebleeding prophylaxis after therapeutic endoscopy in adult patients with liver impairment, no dosage adjustment of the initial 80 mg infusion is necessary. Do not exceed a maximum continuous infusion of esomeprazole 6 mg/h in patients with mild to moderate liver impairment (Child Pugh Classes A and B); and, do not exceed a maximum continuous infusion of 4 mg/h in patients with severe liver impairment (Child Pugh Class C).
No dosage adjustment is necessary. Intermittent hemodialysisNo dosage adjustment is necessary. Due to high protein binding, esomeprazole is not expected to be removed by hemodialysis.
Administer on an empty stomach, at least 60 minutes before meals. If given once daily, administer before the first meal of the day. May be taken during antacid therapy.
Delayed-release capsules (prescription esomeprazole magnesium or strontium capsules): Administer whole, do not crush or chew the delayed-release, enteric-coated granules within the capsule.Alternatively, for patients with difficulty swallowing, the capsule contents can be sprinkled on applesauce. The applesauce should not be hot. Once sprinkled on applesauce, the mixture should be swallowed. Do not chew. Do not store the mixture for future use.An in vitro study indicates that the capsule contents are stable for 30 minutes when suspended in yogurt, cultured milk, apple or orange juice, or tap water. When suspending the contents of a capsule in any of these solid foods or liquids, the mixture should be swallowed without chewing; do not mix and store for future use.Nasogastric (NG) tube administration: The capsules can be opened and the granules emptied into a 60 mL catheter-tipped syringe and mixed with 50 mL of water. It is important to only use a catheter-tipped syringe when administering through a NG tube. Replace the plunger and shake the syringe vigorously for 15 seconds. Hold the syringe with the tip up and check for granules remaining in the tip. Attach the syringe to the NG tube and deliver the contents of the syringe through the tube into the stomach. After administering the granules, the NG tube should be flushed with additional water. Do not administer the granules if they have dissolved or disintegrated. Administer the contents of the syringe immediately; do not store. Delayed-release capsules (non-prescription esomeprazole magnesium capsules; e.g., Nexium 24HR):Administer whole, do not crush or chew the delayed-release capsules; administer with a glass of water, on an empty stomach, in the morning.
Delayed release oral suspension granules:Use the appropriate packet size for the dose to be administered.Patients should not crush or chew the granules. -Administration of a 2.5-mg or 5-mg packet:Empty the contents of packet into a container with 1 teaspoon (5 mL) of water. Stir and leave 2—3 minutes to thicken. Re-stir the mixture before administration; administer within 30 minutes of preparation. Any residual drug left in container should be flushed with more water and administered immediately.Nasogastric (NG) or gastric tube (French size 6 or larger) administration: Add 5 mL of water to a catheter tipped syringe and then add the contents of a 2.5-mg or 5-mg packet. It is important to only use a catheter-tipped syringe when administering through a NG or gastric tube. Immediately shake the syringe and leave 2—3 minutes to thicken. Upon administration, shake the syringe again, and flush the contents through the NG or gastric tube into the stomach; administer within 30 minutes of preparation. Refill the syringe with 5 mL of water, shake to rinse and flush any remaining contents from the NG or gastric tube into the stomach. -Administration of the 10-mg, 20-mg, or 40-mg packet:Empty into a container with 1 tablespoon (15 mL) of water. Stir and leave 2—3 minutes to thicken. Re-stir the mixture before administration; administer within 30 minutes of preparation. Any residual drug left in container should be flushed with more water and administered immediately.Nasogastric (NG) or gastric tube (French size 6 or larger) administration: Add 15 mL of water to a catheter tipped syringe and then add the contents of a 10-mg, 20-mg, or 40-mg packet. It is important to only use a catheter-tipped syringe when administering through a NG or gastric tube. Immediately shake the syringe and leave 2—3 minutes to thicken. Upon administration, shake the syringe again, and flush the contents through the NG or gastric tube into the stomach; administer within 30 minutes of preparation. Refill the syringe with 15 ml of water, shake to rinse and flush any remaining contents from the NG or gastric tube into the stomach.
For intravenous administration only.Visually inspect parenteral products for particulate matter and discoloration prior to administration whenever solution and container permit.
Slow IV Push:IV push administration is indicated for adults only; for pediatric patients use IV infusion administration.Reconstitute the contents of one vial, either 20 mg or 40 mg, with 5 ml of 0.9% Sodium Chloride for Injection (NS).Flush the IV line with either 0.9% Sodium Chloride injection, Lactated Ringer’s, or 5% Dextrose injection both prior to and after administration.Withdraw dose from vial.Administer slowly over no less than 3 minutes.Do NOT administer concomitantly with any other medications through the same IV site and/or tubing.Storage of reconstituted injection: Store at room temperature up to 30 degrees C (86 degrees F) for up to 12 hours when diluted with 0.9% Sodium Chloride injection. Intermittent intravenous (IV) infusion:Reconstitute the contents of 1 vial, either 20 mg or 40 mg, with 5 mL of 0.9% Sodium Chloride injection, 5% Dextrose injection, or Lactated Ringer’s.Prior to administration, further dilute the resulting solution in 50 mL of 0.9% Sodium Chloride injection, 5% Dextrose injection, or Lactated Ringer’s.The final infusion concentrations are 0.8 mg/mL (40 mg/50 mL) or 0.4 mg/mL (20 mg/50 mL).For pediatric patients, withdraw the appropriate volume from the standard infusion preparation to prepare the desired pediatric infusion dose.Flush the IV line with either 0.9% Sodium Chloride injection, Lactated Ringer’s, or 5% Dextrose injection both prior to and after administration.Infuse IV over 10—30 minutes.Do NOT administer concomitantly with any other medications through the same IV site and/or tubing.Storage of infusion solutions: Store at room temperature up to 30 degrees C (86 degrees F). Administer solutions diluted with 0.9% Sodium Chloride injection or Lactated Ringer’s within 12 hours; administer solutions diluted with 5% Dextrose injection within 6 hours. Continuous intravenous (IV) infusion:Reconstitute the contents of 2 x 40 mg vials (80 mg total) with 5 mL of 0.9% Sodium Chloride injection each; further dilute in 100 mL 0.9% Sodium Chloride injection to a final concentration of 0.8 mg/mL for preparation of both the loading dose and separate continuous infusion.After reconstitution, give the 80 mg IV bolus as an IV infusion over a period of 30 minutes.Follow the IV bolus with the continuous infusion at a rate of 8 mg/hour (i.e., 10 mL/hour) for 71.5 hours.Storage of infusion solutions: Store at room temperature up to 30 degrees C (86 degrees F). Administer solutions diluted with 0.9% Sodium Chloride injection within 12 hours.
Generic:- Store between 68 to 77 degrees F, excursions permitted 59 to 86 degrees FNexium:- Store at controlled room temperature (between 68 and 77 degrees F)Nexium 24HR:- Store at controlled room temperature (between 68 and 77 degrees F)
Esomeprazole is contraindicated in patients with known hypersensitivity to esomeprazole or other substituted benzimidazoles such as omeprazole or lansoprazole (i.e., known proton pump inhibitors (PPIs) hypersensitivity). There has been evidence of PPI cross-sensitivity in some sensitive individuals in literature reports. Although rare, occasionally such reactions can be serious (i.e., result in anaphylaxis, angioedema, or acute interstitial nephritis). Esomeprazole is the active isomer of racemic omeprazole; therefore the two drugs should not be taken together as this would constitute duplicative therapy.
Esomeprazole undergoes extensive hepatic metabolism. Patients with severe hepatic disease should receive dose adjustment. No dosage adjustment is recommended in patients with mild to moderate hepatic impairment.
The use of gastric acid suppressive therapy, such as PPIs, may increase the risk of enteric infection by encouraging the growth of gut microflora and increasing susceptibility to organisms including Salmonella, Campylobacter jejuni, Escherichia coli, Clostridium difficile, Vibrio cholerae, and Listeria. A systematic review examined the relationship between PPI use and susceptibility to enteric infections and found enhanced susceptibility for Salmonella infections (adjusted RR range: 4.2—8.3 in 2 studies), Campylobacter (RR 3.5—11.7 in 4 studies) and C. difficile infections (RR 1.2—5.0 in 17 out of 27 studies). In particular, PPI use has been linked to an increased risk of Clostridium difficile–associated diarrhea (CDAD). A diagnosis of CDAD should be considered for patients taking PPIs who develop diarrhea that does not improve. Advise patients to seek immediate care from a healthcare professional if they experience watery stool that does not go away, abdominal pain, and fever while taking PPIs. Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. In addition, PPIs, including esomeprazole, are recommended for use in combination with certain antibiotics to eradicate Helicobacter pylori. Pseudomembranous colitis has been reported with nearly all antibacterial agents and may range in severity from mild to life-threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents in combination with PPIs.
Gastric polyps/fundic gland polyps have been reported during postmarketing surveillance. Patients are usually asymptomatic and fundic gland polyps are identified incidentally on endoscopy. The risk of fundic gland polyps increases with long term proton pump inhibitor (PPI) use, especially beyond one year. Use the shortest duration of PPI therapy appropriate to treat specific condition. Symptomatic response to therapy with esomeprazole does not preclude the presence of gastric cancer or other malignancy.
Daily treatment with gastric acid-suppressing medication such as esomeprazole over a long period of time (e.g., generally >= 2—3 years) may lead to malabsorption of cyanocobalamin and vitamin B12 deficiency. Cases of cyanocobalamin deficiency occurring with acid-suppression therapy have been reported in the literature. One large case-controlled study compared patients with and without an incident diagnosis of vitamin B12 deficiency. A correlation was demonstrated between vitamin B12 deficiency and gastric acid-suppression therapy of > 2 years duration [i.e., proton pump inhibitor (PPI), H2-receptor antagonist]. In addition, a dose-dependant relationship was evident, as larger daily PPI pill counts were more strongly associated with vitamin B12 deficiency. The possibility of cyanocobalamin deficiency should, therefore, be considered if clinical symptoms are observed.
Use proton pump inhibitors (PPIs) in patients with or who have risk factors for osteoporosis cautiously. PPIs have been associated with a possible increased risk of bone fractures of the hip, wrist, and spine. Epidemiological studies have reported an increased risk of fractures with the use of PPIs; the studies compared claims data of patients treated with PPIs versus individuals who were not using PPIs. The risk of fracture was increased in patients who received high-dose (defined as multiple daily doses or doses greater than those recommended in non-prescription use), and long-term PPI therapy (a year or longer); fractures were primarily observed in older adult and geriatric patients 50 years of age and older. It should be noted that pre-approval randomized clinical trials (RCTs) of PPIs have not found an increased risk of fractures of the hip, wrist, or spine; however, these RCTs were of shorter study duration (generally 6 months or less). When prescribing PPIs, consider whether a lower dose or shorter duration of therapy would adequately treat the patient’s condition. In patients with or at risk for osteopenia or osteoporosis, manage their bone status according to current clinical practice, and ensure adequate vitamin D and calcium supplementation. According to the Beers Criteria, PPIs are considered potentially inappropriate medications (PIMs) for use in geriatric patients due to the risk of Clostridium difficile and bone loss/fractures. Scheduled use for more than 8 weeks should be avoided except for high-risk patients (e.g., oral corticosteroids or chronic NSAID use), erosive esophagitis, Barrett’s esophagitis, pathological hypersecretory condition, or demonstrated need for maintenance treatment (e.g., due to failure of drug discontinuation trial or H-2 blockers). The federal Omnibus Budget Reconciliation Act (OBRA) regulates medication use in residents of long-term care facilities (LTCFs). According to the OBRA guidelines, the indication for use of a proton pump inhibitor should be based on clinical symptoms and/or endoscopic findings. During use to treat or prevent NSAID-induced gastritis or esophagitis, there should be documentation that analgesics with less GI toxicity than NSAIDs have been tried or were not indicated. If used for longer than 12 weeks, clinical rationale for continued need and/or documentation should support an underlying chronic disease (e.g., GERD) or risk factors (e.g., chronic NSAID use). Adverse consequences of medication therapy include new or worsening headaches, nausea, emesis, flatulence, difficulty swallowing, abdomen pain, diarrhea, or other GI symptoms. In addition, PPIs may increase the risk of clostridium difficile colitis.
Daily treatment with a gastric acid-suppressing medication over a long period of time (e.g., 3 months to > 1 year) may lead to hypomagnesemia; cases have been reported in patients taking esomeprazole. Generally, hypomagnesemia is corrected with magnesium supplementation; however, in cases where hypomagnesemia is observed during PPI administration, discontinuation of the PPI may also be necessary. Low serum magnesium may lead to serious adverse events such as muscle spasm (tetany), seizures, and irregular heartbeat (arrhythmias). Use PPIs with caution and, if possible, avoid long-term (> 14 days) use in patients with congenital long QT syndrome, as they may be at higher risk for arrhythmias. In pediatric patients, irregular heartbeat may cause fatigue, upset stomach, dizziness, and lightheadedness. For patients expected to be on PPI therapy for a prolonged period of time, it is prudent for clinicians to obtain serum magnesium concentrations prior to initiating PPI therapy as well as throughout treatment. Patients on concomitant medications such as digoxin or diuretics may also require periodic monitoring of serum magnesium.
Studies suggest that long-term PPI therapy is associated with a temporal increase in gastric acid secretion shortly following treatment discontinuation. A similar and well established response has been noted after withdrawal of H2 blockers. Profound gastric acid suppression during PPI therapy leads to a drug-induced reflex hypergastrinemia and subsequent rebound acid hypersecretion. In this hypersecretory state, enterochromaffin-like cell hypertrophy also results in a temporal increase in serum chromogranin A (CgA) levels. It is unclear, however, if this hypersecretory reflex results in clinically significant effects in patients on or attempting to discontinue PPI therapy. A clinically significant effect may lead to gastric acid-related symptoms upon PPI withdrawal and possible therapy dependence. Studies in healthy subjects (H. pylori negative) as well as GERD patients, present conflicting data regarding whether PPI therapy beyond 8-weeks is associated with rebound acid hypersecretion and associated dyspeptic symptoms shortly following PPI cessation. Until more consistent study results shed light on this possible effect, it is prudent to follow current treatment guidelines employing the lowest effective dose, for the shortest duration of time in symptomatic patients. For patients requiring maintenance therapy, consider on demand or intermittent PPI therapy, step down therapy to an H2 blocker, and regularly assess the need for continued gastric suppressive therapy.
There are no adequate and well-controlled studies regarding use of esomeprazole during human pregnancy. Esomeprazole is the S-isomer of omeprazole. Current data, including epidemiologic data and an expert review by TERIS (the Teratogen Information System), fail to demonstrate an increased risk of major congenital malformations or other adverse pregnancy outcomes with first trimester omeprazole use. Animal reproductive studies have been conducted with omeprazole and esomeprazole. Rats and rabbits dosed with omeprazole experienced dose-dependent embryo-lethality at omeprazole doses that were approximately 3.4 to 34 times an oral human dose of 40 mg, based on a body surface area (BSA) for a 60 kg person. Teratogenicity was not observed in animal reproduction studies with administration of oral esomeprazole in rats and rabbits during organogenesis with doses about 68 and 42 times, respectively, an oral human dose of 40 mg esomeprazole or 40 mg omeprazole, based on BSA for a 60 kg person. However, changes in bone morphology were observed in offspring of rats dosed through most of pregnancy and lactation at doses greater than or equal to 33.6 times an oral human dose of 40 mg. Although animal studies are not always predictive of human effects, because of the observed effect at high doses of esomeprazole magnesium on developing bone in rat studies, esomeprazole use in pregnancy should be limited. Esomeprazole, like omeprazole, is expected to cross the human placenta. Epidemiological evaluations have compared the rate of congenital abnormalities and stillbirths among those exposed to omeprazole in utero during pregnancy to similar findings for those exposed to H2-receptor antagonists or other controls. Overall, slightly higher rates of congenital malformations (e.g., ventricular septal defects) and number of stillborns have been reported for cases where exposure to omeprazole occurred in the first trimester of pregnancy and beyond. Use during pregnancy should be limited to cases where the benefit to the mother outweighs any potential risk to the fetus. In 2009, a population-based observational cohort study explored a possible link between gastric acid suppressive therapy (e.g., proton pump inhibitors) during pregnancy and a diagnosis of allergic disease or a prescription for asthma or allergy medications in the exposed child. Among the cohort (n = 585,716), 1% of children exposed to gastric acid suppressive drugs in pregnancy received a diagnosis of allergic disease. For developing allergy or asthma, an increased OR of 1.43 and 1.51, respectively, were observed regardless of drug used, time of exposure during pregnancy, and maternal history of disease. Proposed possible mechanisms for a link include: (1) exposure to increased amounts of allergens could cause sensitization to digestion-labile antigens in the fetus; (2) the maternal Th2 cytokine pattern could promote an allergy prone phenotype in the fetus; (3) maternal allergen specific immunoglobulin could cross the placenta and sensitize fetal immune cells to food and airborne allergens. Study limitations were present and confirmation of results is necessary before further conclusions can be drawn from this data. Risk versus benefit should be considered prior to use. Self-medication with esomeprazole (OTC formulations) during pregnancy is not recommended. Esomeprazole strontium use during pregnancy should only be considered if the potential benefit justifies the potential risk to the fetus. Strontium is known to compete with calcium for intestinal absorption and is incorporated into bone. Because of the effect of esomeprazole strontium observed at high doses on developing bone in animal studies, its use in pediatric patients is not recommended; thus, passage of strontium to a developing fetus is not advisable; alternate therapies should be considered. Pregnant patients should see their health care professional for a proper diagnosis and for treatment recommendations.
Esomeprazole strontium use during breast-feeding should be avoided. Strontium is known to compete with calcium for intestinal absorption and is incorporated into bone. Because of the effect of esomeprazole strontium observed at high doses on developing bone in animal studies, its use in pediatric patients is not recommended; passage to a nursing infant through breast milk should also be avoided. There are no clinical data on the effects of esomeprazole on the nursing infant or on milk production. The developmental and health benefits of breast-feeding should be considered along with the mother’s clinical need for esomeprazole and any potential adverse effects on the nursing infant from esomeprazole or from the underlying maternal condition.Esomeprazole has a low molecular weight (345) and excretion into breast milk is expected. Esomeprazole is the S-isomer of omeprazole and limited data suggest that omeprazole may be present in human milk. One study reported the use of omeprazole in late gestation and continued use through lactation. During breast-feeding, the mother fed her infant prior to a dose of 20 mg of omeprazole. Samples of expressed milk were analyzed and a maximum daily exposure to the infant was calculated to be 4 mcg (based on the consumption of 200 mL of milk/day). Based on the above case, a maximum dose of 3 mcg/kg daily or about 0.9% of the maternal weight-adjusted dosage would be delivered to an exclusively breast-fed infant based on a milk consumption of 150 mL/kg/day. For comparison, doses of 0.5 mg/kg PO once daily for 6 weeks have been studied during infancy (age 2.9 +/- 0.9 months) for peptic esophagitis. Nevertheless, the methods of collection and calculations of the sampled milk were not clearly defined in this case report. Milk expressed early in feeding contains less lipid content as compared to milk expressed towards the end of feeding. Taking into account that omeprazole is a lipid soluble drug, milk expressed and analyzed early on in feeding may not accurately reveal the true exposure to a feeding infant. Potentially serious adverse reactions may occur with the use of omeprazole or esomeprazole during breast-feeding, including suppression of gastric acid secretion in the nursing infant. Alternative therapies for consideration include antacids and H2 blockers. Some experts recommend that consideration of the dose and drug properties may allow for continued nursing without significant exposure to the breast-fed infant for nursing women who require esomeprazole. If possible, the mother should wait to nurse or express milk 5 to 7.5 hours after the daily dose of esomeprazole. Allowing this time should eliminate 97% of the drug from the plasma and would avoid the period when the greatest amount of drug is available to enter the milk. Near the end of the waiting period, breast milk should be expressed and discarded to complete the strategy to limit the infant’s exposure to esomeprazole. This strategy is based on known pharmacokinetic parameters such as half-life; however, further study is warranted examining the use of this strategy in human mother-infant pairs.
The use of the esomeprazole strontium salt is not recommended in neonates, infants, children, and adolescents due to a lack of adequate safety data. Strontium competes with calcium for intestinal absorption and is incorporated into bone; the clinical consequences of use in pediatric patients have not been determined.
The package labeling for non-prescription (OTC) esomeprazole states that patients should not self-medicate with esomeprazole if they have the following: trouble swallowing (dysphagia); vomiting with blood or bloody or black stools (GI bleeding); heartburn with lightheadedness, sweating, or dizziness; chest pain or shoulder pain with shortness of breath, sweating, pain spreading to arms, neck or shoulders, or lightheadedness; or frequent chest pain. Also, a patient should speak with a health care provider prior to using esomeprazole OTC if there is a history of any of the following: heartburn for > 3 months; frequent wheezing, particularly with heartburn; unexplained weight loss; nausea or vomiting; or abdominal pain. Such symptoms may be signs of a serious condition requiring medical evaluation and perhaps prescription therapy.
Use with caution in patients with a history of systemic lupus erythematosus (SLE) as esomeprazole has been reported to activate or exacerbate SLE.
Administration of esomeprazole may result in laboratory test interference, specifically serum chromogranin A (CgA) tests for neuroendocrine tumors, urine tests for tetrahydrocannabinol (THC), secretin stimulation tests, and diagnostic tests for Helicobacter pylori. Gastric acid suppression may increase serum CgA. Increased CgA concentrations may cause false positive results in diagnostic investigations for neuroendocrine tumors. To prevent this interference, temporarily stop esomeprazole at least 14 days before assessing CgA concentrations and consider repeating the test if initial concentrations are high. If serial tests are performed, ensure the same commercial laboratory is used as reference ranges may vary. Reports have suggested use of proton pump inhibitors (PPIs) may cause false positive urine screening tests for THC. If a PPI-induced false positive urine screen is suspected, confirm the positive results using an alternative testing method. PPIs may also cause a hyper-response in gastrin secretion to the secretin stimulation test, falsely suggesting gastrinoma. Health care providers are advised to temporarily stop esomeprazole at least 14 days prior to performing a secretin stimulation test to allow gastrin concentrations to return to baseline. Preparations that combine PPIs with antimicrobials and bismuth are known to suppress H. pylori; thus, ingestion of these preparations within 4 weeks of performing diagnostic tests for H. pylori may lead to false negative results. At a minimum, instruct the patient to avoid the use of esomeprazole in the 1 to 2 weeks prior to the test and the use of antimicrobials and bismuth preparations in the 4 weeks prior to the test.
GI bleeding / Delayed / 0-4.3visual impairment / Early / 0-1.0angioedema / Rapid / 0-1.0pancreatitis / Delayed / Incidence not knowntoxic epidermal necrolysis / Delayed / Incidence not knownanaphylactic shock / Rapid / Incidence not knownStevens-Johnson syndrome / Delayed / Incidence not knownerythema multiforme / Delayed / Incidence not knownanaphylactoid reactions / Rapid / Incidence not knownexfoliative dermatitis / Delayed / Incidence not knownhepatic failure / Delayed / Incidence not knownhepatic encephalopathy / Delayed / Incidence not knowninterstitial nephritis / Delayed / Incidence not knownbronchospasm / Rapid / Incidence not knownagranulocytosis / Delayed / Incidence not knownpancytopenia / Delayed / Incidence not knownlupus-like symptoms / Delayed / Incidence not knownbone fractures / Delayed / Incidence not known
constipation / Delayed / 1.0-2.5candidiasis / Delayed / 0-1.0melena / Delayed / 0-1.0dysphagia / Delayed / 0-1.0stomatitis / Delayed / 0-1.0migraine / Early / 0-1.0blurred vision / Early / 0-1.0confusion / Early / 0-1.0depression / Delayed / 0-1.0hypertonia / Delayed / 0-1.0hyperbilirubinemia / Delayed / 0-1.0elevated hepatic enzymes / Delayed / 0-1.0goiter / Delayed / 0-1.0edema / Delayed / 0-1.0hyponatremia / Delayed / 0-1.0glycosuria / Early / 0-1.0conjunctivitis / Delayed / 0-1.0sinus tachycardia / Rapid / 0-1.0hypertension / Early / 0-1.0chest pain (unspecified) / Early / 0-1.0hyperuricemia / Delayed / 0-1.0peripheral edema / Delayed / 0-1.0dyspnea / Early / 0-1.0hot flashes / Early / 0-1.0anemia / Delayed / 0-1.0thrombocytopenia / Delayed / 0-1.0lymphadenopathy / Delayed / 0-1.0leukopenia / Delayed / 0-1.0hematuria / Delayed / 0-1.0vaginitis / Delayed / 0-1.0cystitis / Delayed / 0-1.0impotence (erectile dysfunction) / Delayed / 0-1.0dysuria / Early / 0-1.0phlebitis / Rapid / Incidence not knownerythema / Early / Incidence not knownhallucinations / Early / Incidence not knownhepatitis / Delayed / Incidence not knownjaundice / Delayed / Incidence not knownvitamin B12 deficiency / Delayed / Incidence not knownpernicious anemia / Delayed / Incidence not knownhypomagnesemia / Delayed / Incidence not knownhypokalemia / Delayed / Incidence not knownhypocalcemia / Delayed / Incidence not knowncolitis / Delayed / Incidence not knownpseudomembranous colitis / Delayed / Incidence not known
headache / Early / 1.9-10.9flatulence / Early / 1.0-10.3dyspepsia / Early / 0-6.4nausea / Early / 1.0-6.4abdominal pain / Early / 1.0-5.8injection site reaction / Rapid / 1.7-4.3diarrhea / Early / 1.0-4.3xerostomia / Early / 1.0-3.9dizziness / Early / 0-2.5drowsiness / Early / 0-1.9sinusitis / Delayed / 1.0-1.7pruritus / Rapid / 0-1.1infection / Delayed / 1.1-1.1eructation / Early / 0-1.0hiccups / Early / 0-1.0weight gain / Delayed / 0-1.0vomiting / Early / 0-1.0weight loss / Delayed / 0-1.0anxiety / Delayed / 0-1.0hypoesthesia / Delayed / 0-1.0parosmia / Delayed / 0-1.0tremor / Early / 0-1.0anorexia / Delayed / 0-1.0paresthesias / Delayed / 0-1.0vertigo / Early / 0-1.0appetite stimulation / Delayed / 0-1.0insomnia / Early / 0-1.0rash / Early / 0-1.0urticaria / Rapid / 0-1.0acne vulgaris / Delayed / 0-1.0maculopapular rash / Early / 0-1.0pruritus ani / Early / 0-1.0diaphoresis / Early / 0-1.0asthenia / Delayed / 0-1.0fever / Early / 0-1.0arthropathy / Delayed / 0-1.0muscle cramps / Delayed / 0-1.0pharyngitis / Delayed / 0-1.0arthralgia / Delayed / 0-1.0cough / Delayed / 0-1.0malaise / Early / 0-1.0flushing / Rapid / 0-1.0rhinitis / Early / 0-1.0back pain / Delayed / 0-1.0fatigue / Early / 0-1.0tinnitus / Delayed / 0-1.0polydipsia / Early / 0-1.0leukocytosis / Delayed / 0-1.0epistaxis / Delayed / 0-1.0increased urinary frequency / Early / 0-1.0polyuria / Early / 0-1.0menstrual irregularity / Delayed / 0-1.0dysmenorrhea / Delayed / 0-1.0gastric polyps / Delayed / Incidence not knownagitation / Early / Incidence not knowndysgeusia / Early / Incidence not knownphotosensitivity / Delayed / Incidence not knownhyperhidrosis / Delayed / Incidence not knownalopecia / Delayed / Incidence not knownweakness / Early / Incidence not knowngynecomastia / Delayed / Incidence not knownmyalgia / Early / Incidence not known
Acalabrutinib: (Major) Avoid the concomitant use of acalabrutinib and proton pump inhibitors (PPI), such as esomeprazole; decreased acalabrutinib exposure may occur resulting in decreased acalabrutinib effectiveness. Consider using an antacid or H2-blocker if acid suppression therapy is needed. Separate the administration of acalabrutinib and antacids by at least 2 hours; give acalabrutinib 2 hours before a H2-blocker. Acalabrutinib solubility decreases with increasing pH values. The AUC of acalabrutinib was decreased by 43% when acalabrutinib was coadministered with another PPI for 5 days. Acetaminophen; Butalbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Acetaminophen; Butalbital; Caffeine: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Acetaminophen; Butalbital; Caffeine; Codeine: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Alendronate: (Moderate) Proton pump inhibitors (PPIs) are widely used and are frequently coadministered in users of oral bisphosphonates. A national register-based, open cohort study of 38,088 elderly patients suggests that those who use proton pump inhibitors in conjunction with alendronate have a dose-dependent loss of protection against hip fracture. While causality was not investigated, the dose-response relationship noted during the study suggested that PPIs may reduce oral alendronate efficacy, perhaps through an effect on absorption or other mechanism, and therefore PPIs may not be optimal agents to control gastrointestinal complaints. It is not yet clear if all bisphosphonates would exhibit a loss of efficacy when PPIs are coadministered, but the results suggest that the interaction may occur across the class. Alendronate; Cholecalciferol: (Moderate) Proton pump inhibitors (PPIs) are widely used and are frequently coadministered in users of oral bisphosphonates. A national register-based, open cohort study of 38,088 elderly patients suggests that those who use proton pump inhibitors in conjunction with alendronate have a dose-dependent loss of protection against hip fracture. While causality was not investigated, the dose-response relationship noted during the study suggested that PPIs may reduce oral alendronate efficacy, perhaps through an effect on absorption or other mechanism, and therefore PPIs may not be optimal agents to control gastrointestinal complaints. It is not yet clear if all bisphosphonates would exhibit a loss of efficacy when PPIs are coadministered, but the results suggest that the interaction may occur across the class. Aliskiren; Amlodipine; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Aliskiren; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Amiloride; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Amlodipine; Hydrochlorothiazide, HCTZ; Olmesartan: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Amlodipine; Hydrochlorothiazide, HCTZ; Valsartan: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Amobarbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Amphetamine: (Moderate) The use of proton pump inhibitors (PPIs) with amphetamine and/or dextroamphetamine therapy may change the onset of action of these amphetamines due to the increase in gastric pH. The time to maximum concentration (Tmax) of amphetamines is decreased compared to when administered alone, thus increasing amphetamine concentrations and exposure, which may be of particular significance with extended-release dosage forms. Monitor clinical response and adjust if needed. Some extended-release dosage forms of amphetamine or dextroamphetamine salts should not be given with PPIs. The concomitant use of PPIs with some extended-release dosage forms may result in amphetamine dose-dumping. Amphetamine; Dextroamphetamine Salts: (Moderate) The use of proton pump inhibitors (PPIs) with amphetamine and/or dextroamphetamine therapy may change the onset of action of these amphetamines due to the increase in gastric pH. The time to maximum concentration (Tmax) of amphetamines is decreased compared to when administered alone, thus increasing amphetamine concentrations and exposure, which may be of particular significance with extended-release dosage forms. Monitor clinical response and adjust if needed. Some extended-release dosage forms of amphetamine or dextroamphetamine salts should not be given with PPIs. The concomitant use of PPIs with some extended-release dosage forms may result in amphetamine dose-dumping. Amphetamine; Dextroamphetamine: (Moderate) The use of proton pump inhibitors (PPIs) with amphetamine and/or dextroamphetamine therapy may change the onset of action of these amphetamines due to the increase in gastric pH. The time to maximum concentration (Tmax) of amphetamines is decreased compared to when administered alone, thus increasing amphetamine concentrations and exposure, which may be of particular significance with extended-release dosage forms. Monitor clinical response and adjust if needed. Some extended-release dosage forms of amphetamine or dextroamphetamine salts should not be given with PPIs. The concomitant use of PPIs with some extended-release dosage forms may result in amphetamine dose-dumping. Ampicillin: (Major) Proton pump inhibitors (PPIs) have long-lasting effects on the secretion of gastric acid. For enteral ampicillin, whose bioavailability is influenced by gastric pH, the concomitant administration of PPIs can exert a significant effect on ampicillin absorption. Ampicillin; Sulbactam: (Major) Proton pump inhibitors (PPIs) have long-lasting effects on the secretion of gastric acid. For enteral ampicillin, whose bioavailability is influenced by gastric pH, the concomitant administration of PPIs can exert a significant effect on ampicillin absorption. Anticholinergics: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Apalutamide: (Major) Avoid coadministration of esomeprazole with apalutamide due to decreased esomeprazole plasma concentrations. Esomeprazole is a CYP3A4 and CYP2C19 substrate. Apalutamide is a strong CYP3A4 and CYP2C19 inducer. Coadministration with another strong inducer of CYP3A4 inducer decreased omeprazole exposure by 37.9% in CYP2C19 poor metabolizers and by 43.9% in extensive metabolizers; esomeprazole is an enantiomer of omeprazole. Aprepitant, Fosaprepitant: (Minor) Use caution if esomeprazole and aprepitant are used concurrently and monitor for an increase in esomeprazole-related adverse effects for several days after administration of a multi-day aprepitant regimen. After administration, fosaprepitant is rapidly converted to aprepitant and shares the same drug interactions. Esomeprazole is a CYP3A4 substrate. Aprepitant, when administered as a 3-day oral regimen (125 mg/80 mg/80 mg), is a moderate CYP3A4 inhibitor and inducer; substitution of fosaprepitant 115 mg IV on day 1 of the 3-day regimen may lessen the inhibitory effects of CYP3A4. The AUC of a single dose of another CYP3A4 substrate, midazolam, increased by 2.3-fold and 3.3-fold on days 1 and 5, respectively, when coadministered with a 5-day oral aprepitant regimen. After a 3-day oral aprepitant regimen, the AUC of midazolam increased by 25% on day 4, and decreased by 19% and 4% on days 8 and 15, respectively, when given on days 1, 4, 8, and 15. As a single 40-mg oral dose, the inhibitory effect of aprepitant on CYP3A4 is weak, with the AUC of midazolam increased by 1.2-fold; the midazolam AUC increased by 1.5-fold after a single 125-mg dose of oral aprepitant. After single doses of IV fosaprepitant, the midazolam AUC increased by 1.8-fold (150 mg) and 1.6-fold (100 mg); less than a 2-fold increase in the midazolam AUC is not considered clinically important. Aspirin, ASA; Butalbital; Caffeine: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Aspirin, ASA; Butalbital; Caffeine; Codeine: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Aspirin, ASA; Carisoprodol: (Minor) Esomeprazole may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as carisoprodol. Carisoprdol is metabolized in the liver by CYP2C19 to form meprobamate. Coadministration may result in increased exposure to carisoprdol and decreased exposure of meprobamate. Aspirin, ASA; Carisoprodol; Codeine: (Minor) Esomeprazole may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as carisoprodol. Carisoprdol is metabolized in the liver by CYP2C19 to form meprobamate. Coadministration may result in increased exposure to carisoprdol and decreased exposure of meprobamate. Atazanavir: (Severe) Coadministration of proton pump inhibitors (PPIs) with atazanavir in treatment-experienced patients is contraindicated. PPIs can be used with atazanavir in treatment-naive patients under specific administration restrictions. In treatment-naive patients >= 40 kg, the PPI dose should not exceed the equivalent of omeprazole 20 mg/day, and the PPI must be administered 12 hours before atazanavir and ritonavir; use the dosage regimen of atazanavir 300 mg boosted with ritonavir 100 mg given once daily with food. While data are insufficient to recommend atazanavir dosing in children Atazanavir; Cobicistat: (Severe) Coadministration of proton pump inhibitors (PPIs) with atazanavir in treatment-experienced patients is contraindicated. PPIs can be used with atazanavir in treatment-naive patients under specific administration restrictions. In treatment-naive patients >= 40 kg, the PPI dose should not exceed the equivalent of omeprazole 20 mg/day, and the PPI must be administered 12 hours before atazanavir and ritonavir; use the dosage regimen of atazanavir 300 mg boosted with ritonavir 100 mg given once daily with food. While data are insufficient to recommend atazanavir dosing in children Atenolol; Chlorthalidone: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Atovaquone; Proguanil: (Moderate) Esomeprazole may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as proguanil. Monitor the patient for common proguanil side effects, such as nausea or other stomach and intestinal complaints, headache, or increased hepatic enzymes when proguanil is given chronically. Atropine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Atropine; Benzoic Acid; Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Atropine; Difenoxin: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Atropine; Diphenoxylate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Atropine; Edrophonium: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Atropine; Hyoscyamine; Phenobarbital; Scopolamine: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Azilsartan; Chlorthalidone: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Barbiturates: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Belladonna Alkaloids; Ergotamine; Phenobarbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Belladonna; Opium: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Benazepril; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Bendroflumethiazide; Nadolol: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Benzoic Acid; Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Benztropine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Bisacodyl: (Minor) The concomitant use of bisacodyl oral tablets with drugs that raise gastric pH like proton pump inhibitors can cause the enteric coating of the bisacodyl tablets to dissolve prematurely, leading to possible gastric irritation or dyspepsia. When taking bisacodyl tablets, it is advisable to avoid PPIs within 1 hour before or after the bisacodyl dosage. Bisoprolol; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Boceprevir: (Moderate) Close clinical monitoring is advised when administering esomeprazole with boceprevir due to an increased potential for esomeprazole-related adverse events. If esomeprazole dosage adjustments are made, re-adjust the dose upon completion of boceprevir treatment. Although this interaction has not been studied, predictions about the interaction can be made based on the metabolic pathway of esomeprazole. Esomeprazole is partially metabolized by the hepatic isoenzyme CYP3A4; boceprevir inhibits this isoenzyme. Coadministration may result in elevated esomeprazole plasma concentrations. Bortezomib: (Minor) Bortezomib may inhibit CYP2C19 activity at therapeutic concentrations and increase exposure to drugs that are substrates for this enzyme including proton pump inhibitors. Bosentan: (Moderate) Monitor for decreased efficacy of esomeprazole if coadministration with bosentan is necessary. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Bosentan is a moderate CYP3A4 inducer. Drugs known to induce CYP3A4 may lead to decreased esomeprazole plasma concentrations. The manufacturer of esomeprazole recommends avoidance with strong inducers because decreased exposure of esomeprazole can occur. Recommendations are not available for concomitant use with moderate inducers of CYP3A4. Bosutinib: (Major) Bosutinib displays pH-dependent aqueous solubility; therefore, concomitant use of bosutinib and proton-pump inhibitors, such as esomeprazole, may result in decreased plasma exposure of bosutinib. Consider using a short-acting antacid or H2 blocker if acid suppression therapy is needed; separate the administration of bosutinib and antacids or H2-blockers by more than 2 hours. Budesonide: (Minor) Enteric-coated budesonide granules dissolve at a pH greater than 5.5. Concomitant use of budesonide oral capsules and drugs that increase gastric pH levels can cause the coating of the granules to dissolve prematurely, possibly affecting release properties and absorption of the drug in the duodenum. Budesonide; Formoterol: (Minor) Enteric-coated budesonide granules dissolve at a pH greater than 5.5. Concomitant use of budesonide oral capsules and drugs that increase gastric pH levels can cause the coating of the granules to dissolve prematurely, possibly affecting release properties and absorption of the drug in the duodenum. Bumetanide: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with loop diuretics (furosemide, bumetanide, torsemide, and ethacrynic acid). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Butabarbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Calcium Carbonate; Risedronate: (Major) Use of proton pump inhibitors (PPIs) with delayed-release risedronate tablets (Atelvia) is not recommended. Co-administration of drugs that raise stomach pH increases risedronate bioavailability due to faster release of the drug from the enteric coated tablet. This interaction does not apply to risedronate immediate-release tablets. In healthy subjects who received esomeprazole for 6 days, the Cmax and AUC of a single dose of risedronate delayed-release tablets (Atelvia) increased by 60% and 22%, respectively. PPIsare widely used and are frequently coadministered in users of oral bisphosphonates. A national register-based, open cohort study of 38,088 elderly patients suggests that those who use PPIs in conjunction with alendronate have a dose-dependent loss of protection against hip fracture. While causality was not investigated, the dose-response relationship noted during the study suggested that PPIs may reduce oral alendronate efficacy, perhaps through an effect on absorption or other mechanism, and therefore PPIs may not be optimal agents to control gastrointestinal complaints. Study results suggest that the interaction may occur across the class; however, other interactions have not been confirmed and data suggest that fracture protection is not diminished when risedronate is used with PPIs. A post hoc analysis of patients who took risedronate 5 mg daily during placebo-controlled clinical trials determined that risedronate significantly reduced the risk of new vertebral fractures compared to placebo, regardless of concomitant PPI use. PPI users (n = 240) and PPI non-users (n = 2489) experienced fracture risk reductions of 57% (p = 0.009) and 38% (p Candesartan; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Cannabidiol: (Moderate) Consider a dose reduction of cannabidiol if coadministered with esomeprazole. Coadministration may increase cannabidiol plasma concentrations increasing the risk of adverse reactions. Cannabidiol is metabolized by CYP2C19; esomeprazole is a moderate inhibitor of CYP2C19. Capecitabine: (Moderate) Use caution if treatment with a proton pump inhibitor (PPI) is necessary in patients taking capecitabine, as progression-free survival (PFS) and overall survival (OS) may be adversely affected. The mechanism of this potential interaction is unknown and data are conflicting. In a posthoc, retrospective, subgroup analysis of a phase 3 clinical trial in patients with advanced or metastatic gastroesophageal cancer, administration of a PPI was associated with a significant decrease in PFS and OS in patients treated with capecitabine plus oxaliplatin (CapeOx) vs. patients who did not receive a PPI; a significant difference was not observed in the CapeOx plus lapatinib arm. Demographically, there were significantly more Asian patients in the PPI arm of this analysis; according to the manufacturer of capecitabine, Japanese patients have a 36% lower Cmax and 24% lower AUC for capecitabine compared with Caucasian patients. Additionally, there was not a significant increase in concentration dependent toxicities (e.g., hand-foot syndrome, rash, and diarrhea) or dose reductions in either arm. These observations are in line with a previous retrospective study in which patients with colorectal cancer receiving PPI treatment and adjuvant capecitabine also experienced poorer relapse-free survival compared with patients not receiving a PPI. Coadministration with antacids increased exposure to capecitabine and its metabolites, but this was not clinically significant or clinically relevant. Pharmacokinetic data on the impact of a PPI on capecitabine exposure are not available. Captopril; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Carbamazepine: (Moderate) Coadministration may result in increased carbamazepine serum concentrations and decreased esomeprazole serum concentrations. Carbamazepine induces cytochrome P-450 enzymes, including those responsible for the metabolism of esomeprazole possibly resulting in reduced esomeprazole concentrations. Some manufacturers recommend avoiding the coadministration of hepatic cytochrome P-450 enzyme inducers and proton pump inhibitors (PPIs). A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If carbamazepine and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. In addition, in one study, multiple dose administration of another PPI, omeprazole, increased the Cmax, AUC, and elimination half-life of carbamazepine when given as an extended-release formulation in healthy male volunteers. Based on these results, it would be prudent to monitor carbamazepine serum concentrations when esomeprazole is added to the drug regimen. Carisoprodol: (Minor) Esomeprazole may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as carisoprodol. Carisoprdol is metabolized in the liver by CYP2C19 to form meprobamate. Coadministration may result in increased exposure to carisoprdol and decreased exposure of meprobamate. Cefpodoxime: (Moderate) Cefpodoxime proxetil requires a low gastric pH for dissolution; therefore, concurrent administration with medications that increase gastric pH, such as proton pump inhibitors (PPIs) may decrease the bioavailability of cefpodoxime. When cefpodoxime was administered with high doses of antacids and H2-blockers, peak plasma concentrations were reduced by 24% and 42% and the extent of absorption was reduced by 27% and 32%, respectively. The rate of absorption is not affected. Ceftibuten: (Minor) Coadministration of 150 mg of ranitidine every 12 hours for 3 days increased the ceftibuten Cmax by 23 percent and ceftibuten AUC by 16 percent. Based on this information, increased gastric pH caused by PPIs may possibly affect the kinetics of ceftibuten. Cefuroxime: (Major) Avoid the concomitant use of proton pump inhibitors (PPIs) and cefuroxime. Drugs that reduce gastric acidity, such as PPIs, can interfere with the oral absorption of cefuroxime axetil and may result in reduced antibiotic efficacy. Chlordiazepoxide; Clidinium: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Chlorothiazide: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Chlorthalidone: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Chlorthalidone; Clonidine: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Cilostazol: (Major) Cilostazol is metabolized by the CYP2C19 hepatic isoenzyme and appears to have pharmacokinetic interactions with many medications that are potent inhibitors of CYP2C19, such as esomeprazole. When given concurrently with omeprazole, another CYP2C19 inhibitor, cilostazol AUC is increased by 26% and the Cmax is increased by 18%; the AUC of the active metabolite 3,4-dehydro-cilostazol is increased by 69% and the Cmax is increased by 29%. When administered concomitantly with esomeprazole, the cilostazol dosage should be reduced by 50%. Ciprofloxacin: (Minor) Use caution when administering ciprofloxacin and esomeprazole concurrently. Ciprofloxacin is an inhibitor of CYP3A, and esomeprazole is partially metabolized by CYP3A. Coadministration of ciprofloxacin with CYP3A substrates, such as esomeprazole, can theoretically increase esomeprazole exposure leading to increased or prolonged therapeutic effects and adverse events; however, the clinical impact of this has not yet been determined. Citalopram: (Moderate) Esomeprazole, a CYP2C19 inhibitor, may iincrease concentrations of citalopram, which may increase the risk for QT prolongation or serotonin side effects.The maximum daily dose of citalopram should not exceed 20 mg per day in patients receiving CYP2C19 inhibitors. Monitor the patient for serotonin excess or symptoms of other citalopram-related side effects. In one study, citalopram concentrations were significantly higher in patients treated with esomeprazole (increased 32.8%). Clobazam: (Moderate) Coadministration may increase serum concentrations of clobazam; a dosage reduction of clobazam may be necessary during coadministration of esomeprazole. Metabolism of N-desmethylclobazam, the active metabolite of clobazam, occurs primarily through CYP2C19 and esomeprazole is an inhibitor of CYP2C19. Extrapolation from pharmacogenomic data indicates that concurrent use of clobazam with moderate or potent inhibitors of CYP2C19 may result in up to a 5-fold increase in exposure to N-desmethylclobazam. Adverse effects, such as sedation, lethargy, ataxia, or insomnia may be potentiated. Clomipramine: (Minor) Esomeprazole may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as clomipramine. Clopidogrel: (Major) Avoid concomitant use of clopidogrel and esomeprazole as it significantly reduces the antiplatelet activity of clopidogrel. If necessary, consider using a PPI medication with less pronounced effects on antiplatelet activity, such as rabeprazole, pantoprazole, lansoprazole, or dexlansoprazole. Clopidogrel requires hepatic biotransformation via 2 cytochrome dependent oxidative steps; the CYP2C19 isoenzyme is involved in both steps. Esomeprazole is an inhibitor of CYP2C19. In clinical studies, use of esomeprazole significantly reduced the antiplatelet activity of clopidogrel. Cobicistat: (Minor) Use caution when administering cobicistat and esomeprazole concurrently. Cobicistat is an inhibitor of CYP3A, and esomeprazole is partially metabolized by CYP3A. Coadministration of cobicistat with CYP3A substrates, such as esomeprazole, can theoretically increase esomeprazole exposure leading to increased or prolonged therapeutic effects and adverse events; however, the clinical impact of this has not yet been determined. Cyanocobalamin, Vitamin B12: (Moderate) Proton pump inhibitors may cause a decrease in the oral absorption of cyanocobalamin, vitamin B12. Patients receiving long-term therapy with proton pump inhibitors should be monitored for signs of B12 deficiency. Cysteamine: (Major) Monitor white blood cell (WBC) cystine concentration closely when administering delayed-release cysteamine (Procysbi) with proton pump inhibitors (PPIs). Drugs that increase the gastric pH may cause the premature release of cysteamine from delayed-release capsules, leading to an increase in WBC cystine concentration. Concomitant administration of omeprazole 20 mg did not alter the pharmacokinetics of delayed-release cysteamine when administered with orange juice; however, the effect of omeprazole on the pharmacokinetics of delayed-release cysteamine when administered with water have not been studied. Dacomitinib: (Major) Avoid coadministration of esomeprazole with dacomitinib due to decreased plasma concentrations of dacomitinib which may impact efficacy. Coadministration with another proton pump inhibitor decreased the dacomitinib Cmax and AUC by 51% and 39%, respectively. Darunavir; Cobicistat: (Minor) Use caution when administering cobicistat and esomeprazole concurrently. Cobicistat is an inhibitor of CYP3A, and esomeprazole is partially metabolized by CYP3A. Coadministration of cobicistat with CYP3A substrates, such as esomeprazole, can theoretically increase esomeprazole exposure leading to increased or prolonged therapeutic effects and adverse events; however, the clinical impact of this has not yet been determined. Darunavir; Cobicistat; Emtricitabine; Tenofovir alafenamide: (Minor) Use caution when administering cobicistat and esomeprazole concurrently. Cobicistat is an inhibitor of CYP3A, and esomeprazole is partially metabolized by CYP3A. Coadministration of cobicistat with CYP3A substrates, such as esomeprazole, can theoretically increase esomeprazole exposure leading to increased or prolonged therapeutic effects and adverse events; however, the clinical impact of this has not yet been determined. Dasabuvir; Ombitasvir; Paritaprevir; Ritonavir: (Moderate) Concurrent administration of esomeprazole with ritonavir may result in elevated esomeprazole plasma concentrations. Esomeprazole is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Monitor patients for increased side effects if these drugs are administered together. Dasatinib: (Major) Do not administer proton pump inhibitors with dasatinib due to the potential for decreased dasatinib exposure and reduced efficacy. Consider using an antacid if acid suppression therapy is needed. Administer the antacid at least 2 hours prior to or 2 hours after the dose of dasatinib. Concurrent use of an proton pump inhibitor reduced the mean Cmax and AUC of dasatinib by 42% and 43%, respectively. Delavirdine: (Major) Because proton pump inhibitors (PPIs) increase gastric pH, decreased delavirdine absorption may occur. However, since these agents affect gastric pH for an extended period, separation of doses may not eliminate the interaction. Chronic use of PPIs with delavirdine is not recommended. Dexamethasone: (Moderate) Monitor for decreased efficacy of esomeprazole if coadministration with dexamethasone is necessary. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Dexamethasone is a moderate CYP3A4 inducer. Drugs known to induce CYP3A4 may lead to decreased esomeprazole plasma concentrations. The manufacturer of esomeprazole recommends avoidance with strong inducers because decreased exposure of esomeprazole can occur. Recommendations are not available for concomitant use with moderate inducers of CYP3A4. Dexmethylphenidate: (Minor) The effects of gastrointestinal pH alterations on the absorption of extended-release dexmethylphenidate (Focalin XR) have not been studied. Per the manufacturer of extended-release dexmethylphenidate, the modified release characteristics are pH-dependent. It is possible that the administration of proton pump inhibitors (PPIs) or other acid suppressants could alter the release of extended-release dexmethylphenidate, resulting in reduced or increased absorption. Patients receiving a PPI should be monitored for adverse effects and reduced therapeutic efficacy of extended-release dexmethylphenidate. Dextroamphetamine: (Moderate) The use of proton pump inhibitors (PPIs) with amphetamine and/or dextroamphetamine therapy may change the onset of action of these amphetamines due to the increase in gastric pH. The time to maximum concentration (Tmax) of amphetamines is decreased compared to when administered alone, thus increasing amphetamine concentrations and exposure, which may be of particular significance with extended-release dosage forms. Monitor clinical response and adjust if needed. Some extended-release dosage forms of amphetamine or dextroamphetamine salts should not be given with PPIs. The concomitant use of PPIs with some extended-release dosage forms may result in amphetamine dose-dumping. Diazepam: (Moderate) Diazepam is a substrate for the CYP2C19 isozyme. Since esomeprazole is an inhibitor of the CYP2C19 isozyme, plasma levels of diazepam may increase. Administration of esomeprazole with diazepam resulted in a 45% reduced clearance of diazepam. According to the manufacturer, this interaction is not likely to be clinically relevant. However, it would be prudent to monitor patients more closely, particularly if other CNS depressants are prescribed. The manufacturer reports that use of diazepam does not appear to alter the pharmacokinetic profile of esomeprazole. Dicyclomine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Digoxin: (Moderate) Increased serum digoxin concentrations have been reported in patients who received digoxin and esomeprazole. Esomeprazole inhibits gastric acid secretion and increases the pH of the stomach. Changes in intragastric pH can potentially alter the bioavailability of other drugs with pH-dependent absorption, such as digoxin. Gastric acid pump-inhibitors may increase digoxin bioavailability; however, the magnitude of the interaction is small. Measure serum digoxin concentrations before initiating esomeprazole. Monitor patients for possible digoxin toxicity and reduce digoxin dose as necessary. In addition, proton pump inhibitors have been associated with hypomagnesemia. Because, low serum magnesium may lead to irregular heartbeat and increase the likelihood of serious arrhythmias, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and digoxin concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Dolutegravir; Rilpivirine: (Severe) Concurrent use of proton pump inhibitors and rilpivirine is contraindicated; when these drugs are coadministered, there is a potential for treatment failure and/or the development of rilpivirine or NNRTI resistance. Proton pump inhibitors inhibit secretion of gastric acid by proton pumps thereby increasing the gastric pH; for optimal absorption, rilpivirine requires an acidic environment. Coadministration of a proton pump inhibitor and rilpivirine may result in decreased rilpivirine absorption/serum concentrations, which could cause impaired virologic response to rilpivirine. Dronedarone: (Moderate) Dronedarone is metabolized by and is an inhibitor of CYP3A. Esomeprazole is a substrate for CYP3A4. The concomitant administration of dronedarone and CYP3A substrates may result in increased exposure of the substrate and should, therefore, be undertaken with caution. Efavirenz: (Minor) Although drug interaction studies have not been conducted, efavirenz may inhibit the metabolism of substrates for CYP2C9 or CYP2C19 such as esomeprazole. In vitro studies have shown that efavirenz inhibits CYP2C9 and CYP2C19 in the range of observed efavirenz plasma concentrations. Efavirenz; Emtricitabine; Tenofovir: (Minor) Although drug interaction studies have not been conducted, efavirenz may inhibit the metabolism of substrates for CYP2C9 or CYP2C19 such as esomeprazole. In vitro studies have shown that efavirenz inhibits CYP2C9 and CYP2C19 in the range of observed efavirenz plasma concentrations. Efavirenz; Lamivudine; Tenofovir Disoproxil Fumarate: (Minor) Although drug interaction studies have not been conducted, efavirenz may inhibit the metabolism of substrates for CYP2C9 or CYP2C19 such as esomeprazole. In vitro studies have shown that efavirenz inhibits CYP2C9 and CYP2C19 in the range of observed efavirenz plasma concentrations. Elvitegravir; Cobicistat; Emtricitabine; Tenofovir Alafenamide: (Minor) Use caution when administering cobicistat and esomeprazole concurrently. Cobicistat is an inhibitor of CYP3A, and esomeprazole is partially metabolized by CYP3A. Coadministration of cobicistat with CYP3A substrates, such as esomeprazole, can theoretically increase esomeprazole exposure leading to increased or prolonged therapeutic effects and adverse events; however, the clinical impact of this has not yet been determined. Elvitegravir; Cobicistat; Emtricitabine; Tenofovir Disoproxil Fumarate: (Minor) Use caution when administering cobicistat and esomeprazole concurrently. Cobicistat is an inhibitor of CYP3A, and esomeprazole is partially metabolized by CYP3A. Coadministration of cobicistat with CYP3A substrates, such as esomeprazole, can theoretically increase esomeprazole exposure leading to increased or prolonged therapeutic effects and adverse events; however, the clinical impact of this has not yet been determined. Emtricitabine; Rilpivirine; Tenofovir alafenamide: (Severe) Concurrent use of proton pump inhibitors and rilpivirine is contraindicated; when these drugs are coadministered, there is a potential for treatment failure and/or the development of rilpivirine or NNRTI resistance. Proton pump inhibitors inhibit secretion of gastric acid by proton pumps thereby increasing the gastric pH; for optimal absorption, rilpivirine requires an acidic environment. Coadministration of a proton pump inhibitor and rilpivirine may result in decreased rilpivirine absorption/serum concentrations, which could cause impaired virologic response to rilpivirine. Emtricitabine; Rilpivirine; Tenofovir disoproxil fumarate: (Severe) Concurrent use of proton pump inhibitors and rilpivirine is contraindicated; when these drugs are coadministered, there is a potential for treatment failure and/or the development of rilpivirine or NNRTI resistance. Proton pump inhibitors inhibit secretion of gastric acid by proton pumps thereby increasing the gastric pH; for optimal absorption, rilpivirine requires an acidic environment. Coadministration of a proton pump inhibitor and rilpivirine may result in decreased rilpivirine absorption/serum concentrations, which could cause impaired virologic response to rilpivirine. Enalapril; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Enzalutamide: (Major) Avoid coadministration of esomeprazole with enzalutamide due to decreased esomeprazole plasma concentrations. Esomeprazole is a CYP3A4 and CYP2C19 substrate. Enzalutamide is a strong CYP3A4 inducer and a moderate CYP2C19 inducer. Coadministration with another strong inducer of CYP3A4 inducer decreased omeprazole exposure by 37.9% in CYP2C19 poor metabolizers and by 43.9% in extensive metabolizers; esomeprazole is an enantiomer of omeprazole. Eprosartan; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Erlotinib: (Major) Avoid coadministration of erlotinib with esomeprazole if possible due to decreases in erlotinib plasma concentrations. Erlotinib solubility is pH dependent and solubility decreases as pH increases. Coadministration of erlotinib with medications that increase the pH of the upper gastrointestinal tract may decrease the absorption of erlotinib. Separation of doses may not eliminate the interaction since proton pump inhibitors affect the pH of the upper GI tract for an extended period of time. Increasing the dose of erlotinib is also not likely to compensate for the loss of exposure. Coadministration with another proton pump inhibitor decreased erlotinib exposure by 46% and the erlotinib Cmax by 61%. Escitalopram: (Moderate) Monitor for serotonin excess or symptoms of other escitalopram-related side effects during coadministration of esomeprazole. Esomeprazole, a CYP2C19 inhibitor, may increase concentrations of escitalopram, which may increase the risk for side effects. In one study, escitalopram concentrations were significantly higher (increased 81.8%) in patients treated with esomeprazole. Eslicarbazepine: (Moderate) Eslicarbazepine may inhibit the CYP2C19-mediated and induce the CYP3A4-mediated metabolism of esomeprazole; both enzymes are involved in the metabolism of esomeprazole. It is unclear that the theoretical interaction would result in a net increase or decrease in PPI action. Some manufacturers recommend avoiding the coadministration of hepatic cytochrome P-450 enzyme inducers and PPIs. If eslicarbazepine and PPI must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy, or for signs of PPI side effects. Ethacrynic Acid: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with loop diuretics (furosemide, bumetanide, torsemide, and ethacrynic acid). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Felbamate: (Minor) Felbamate may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Flavoxate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Flibanserin: (Major) The concomitant use of flibanserin and strong CYP2C19 inhibitors, such as proton pump inhibitors (PPIs), may increase flibanserin concentrations, resulting in severe hypotension, syncope, and/or CNS depression. Therefore, patients should be monitored for flibanserin-induced adverse reactions, and the risks of combination therapy should be discussed with the patient. In addition, the concomitant use of flibanserin and multiple weak CYP3A4 inhibitors, including pantoprazole, may increase flibanserin concentrations, which may increase the risk of flibanserin-induced adverse reactions. Fluconazole: (Minor) Fluconazole may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Fluoxetine: (Minor) Fluoxetine may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Fluoxetine; Olanzapine: (Minor) Fluoxetine may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Fluvastatin: (Moderate) Concomitant administration of cimetidine, ranitidine, or omeprazole with fluvastatin can decrease fluvastatin clearance by 18 to 23%, and increase AUC by 24 to 33%. A similar interaction might be expected with esomeprazole. Fluvoxamine: (Minor) Fluvoxamine may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Fosinopril; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Fosphenytoin: (Moderate) Esomeprazole, which is an inhibitor of CYP2C19, may lead to increased levels of fosphenytoin, a substrate of CYP2C19. During clinical drug interaction studies, the changes in phenytoin concentrations appeared unlikely to be of clinical significance for most patients. However, it is advisable to monitor phenytoin levels and for hydantoin toxicity during concurrent treatment. Drugs known to induce CYP2C19 or CYP3A4 or both, such as fosphenytoin, may lead to decreased esomeprazole serum levels and patients should be monitored for expected clinical benefit during PPI treatment. Furosemide: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with loop diuretics (furosemide, bumetanide, torsemide, and ethacrynic acid). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Gefitinib: (Major) Avoid coadministration of esomeprazole with gefitinib if possible due to decreased exposure to gefitinib, which may lead to reduced efficacy. If concomitant use is unavoidable, take gefitinib 12 hours after the last dose or 12 hours before the next dose of esomeprazole. Gefitinib exposure is affected by gastric pH. Coadministration with another drug to maintain gastric pH above 5 decreased gefitinib exposure by 47%. Glycopyrrolate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Glycopyrrolate; Formoterol: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Homatropine; Hydrocodone: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Hydralazine; Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Irbesartan: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Lisinopril: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Losartan: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Methyldopa: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Metoprolol: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Moexipril: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Olmesartan: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Propranolol: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Quinapril: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Spironolactone: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Telmisartan: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Triamterene: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hydrochlorothiazide, HCTZ; Valsartan: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Hyoscyamine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate; Sodium Biphosphate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Idelalisib: (Major) Avoid concomitant use of idelalisib, a strong CYP3A inhibitor, with esomeprazole, a CYP3A substrate, as esomeprazole toxicities may be significantly increased. The AUC of a sensitive CYP3A substrate was increased 5.4-fold when coadministered with idelalisib. Imipramine: (Minor) In the hepatic oxidative system, esomeprazole is metabolized primarily by CYP2C19 and secondarily by the CYP3A4 isoenzyme. Theoretically, esomeprazole may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as imipramine. Indacaterol; Glycopyrrolate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Iron: (Major) The bioavailability of oral iron salts is influenced by gastric pH, and the concomitant administration of proton pump inhibitors can decrease iron absorption. The non-heme ferric form of iron needs an acidic intragastric pH to be reduced to ferrous and to be absorbed. Iron salts and polysaccharide-iron complex provide non-heme iron. Proton pump inhibitors have long-lasting effects on the secretion of gastric acid and thus, increase the pH of the stomach. The increase in intragastric pH can interfere with the absorption of iron salts. Isavuconazonium: (Moderate) Concomitant use of isavuconazonium with esomeprazole may result in increased concentrations of esomeprazole. Esomeprazole is a substrate of the hepatic isoenzyme CYP3A4; isavuconazole, the active moiety of isavuconazonium, is a moderate inhibitor of this enzyme. Caution and close monitoring are advised if these drugs are used together. Isoniazid, INH: (Minor) Isoniazid, INH may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Isoniazid, INH; Pyrazinamide, PZA; Rifampin: (Major) Some manufacturers recommend avoiding the coadministration of rifampin and proton pump inhibitors (PPIs). Rifamycins induce multiple hepatic cytochrome P-450 enzymes, including those responsible for the metabolism of PPIs. A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If rifampin and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. (Minor) Isoniazid, INH may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Isoniazid, INH; Rifampin: (Major) Some manufacturers recommend avoiding the coadministration of rifampin and proton pump inhibitors (PPIs). Rifamycins induce multiple hepatic cytochrome P-450 enzymes, including those responsible for the metabolism of PPIs. A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If rifampin and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. (Minor) Isoniazid, INH may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Itraconazole: (Moderate) When administering proton pump inhibitors with the 100 mg itraconazole capsule and 200 mg itraconazole tablet formulations, systemic exposure to itraconazole is decreased. Conversely, exposure to itraconazole is increased when proton pump inhibitors are administered with the 65 mg itraconazole capsule. Administer proton pump inhibitors at least 2 hours before or 2 hours after the 100 mg capsule or 200 mg tablet. Monitor for increased itraconazole-related adverse effects if proton pump inhibitors are administered with itraconazole 65 mg capsules. Ketoconazole: (Major) Because ketoconazole requires an acidic pH for absorption, coadministration of a proton pump inhibitor (PPI) with ketoconazole can cause a notable decrease in the bioavailability of ketoconazole. PPIs have a prolonged duration of action, and staggering their time of administration with ketoconazole by several hours may not prevent the drug interaction. An alternative imidazole antifungal should be chosen if any of these gastrointestinal medications are required. If these drugs must be coadministered, administer ketoconazole tablets with an acidic beverage and closely monitor for breakthrough infection. Ledipasvir; Sofosbuvir: (Major) Solubility of ledipasvir decreases as gastric pH increases; thus, coadministration of ledipasvir; sofosbuvir with proton pump inhibitors (PPIs) may result in lower ledipasvir plasma concentrations. Ledipasvir can be administered with PPIs if given simultaneously under fasting conditions. The PPI dose should not exceed a dose that is comparable to omeprazole 20 mg/day. Loop diuretics: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with loop diuretics (furosemide, bumetanide, torsemide, and ethacrynic acid). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Lopinavir; Ritonavir: (Moderate) Concurrent administration of esomeprazole with ritonavir may result in elevated esomeprazole plasma concentrations. Esomeprazole is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Monitor patients for increased side effects if these drugs are administered together. Luliconazole: (Minor) Theoretically, luliconazole may increase the side effects of esomeprazole, which is a CYP2C19 and a CYP3A4 substrate. Monitor patients for adverse effects of exomeprazole, such as GI events. In vitro, therapeutic doses of luliconazole inhibit the activity of CYP2C19 and CYP3A4 and small systemic concentrations may be noted with topical application, particularly when applied to patients with moderate to severe tinea cruris. No in vivo drug interaction trials were conducted prior to the approval of luliconazole. Lumacaftor; Ivacaftor: (Moderate) Lumacaftor; ivacaftor may reduce the efficacy of esomeprazole by substantially decreasing its systemic exposure. If used together, an esomeprazole dosage adjustment may be necessary to obtain the desired therapeutic effect. Esomeprazole is a CYP3A4 and CYP2C19 substrate. Lumacaftor; ivacaftor is a strong inducer of CYP3A; in vitro data suggests is also has the potential to induce CYP2C19. Mefloquine: (Moderate) Proton pump inhibitors (PPIs) may increase plasma concentrations of mefloquine. Patients on chronic mefloquine therapy might be at increased risk of adverse reactions, especially patients with a neurological or psychiatric history. Mepenzolate: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Mephobarbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Mesalamine, 5-ASA: (Major) The dissolution of the coating on mesalamine extended-release capsules (Apriso) and the delayed-release tablets (Lialda) is dependent on pH. Avoid coadministration with drugs that raise gastric pH like proton pump inhibitors. Methenamine; Sodium Acid Phosphate; Methylene Blue; Hyoscyamine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Methohexital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Methotrexate: (Major) Use caution when administering high-dose methotrexate to patients receiving proton pump inhibitors (PPIs); a temporary withdrawal of the PPI should be considered in some patients receiving high-dose methotrexate. Case reports and published population pharmacokinetic studies suggest that concomitant use of some PPIs such as omeprazole, pantoprazole, or esomeprazole with methotrexate primarily at high dose may elevate and prolong serum methotrexate concentrations and/or its metabolite hydroxymethotrexate, which may lead to methotrexate toxicities. In two of these cases, delayed methotrexate elimination was observed when high-dose methotrexate was coadministered with PPIs but was not observed when methotrexate was coadministered with ranitidine. However, no formal drug interaction studies of methotrexate with ranitidine have been conducted. Among adults who received high-dose methotrexate (median dose of 3500 mg/m2, range of 1000-5000 mg/m2), coadministration of PPIs such as omeprazole, lansoprazole, or rabeprazole was identified as a risk factor for delayed methotrexate elimination with an OR of 2.65 (95% confidence interval 1.036.82). The interaction may be partially explained by the inhibitory effects of PPIs on breast cancer resistance protein (BCRP, ABCG2) -mediated methotrexate transport. Altered methotrexate elimination may not be present or problematic among patients who receive lower methotrexate doses. For example, coadministration of lansoprazole 30 mg daily and naproxen 500 mg twice daily for 7 days to recipients of stable oral methotrexate doses (7.515 mg/week) for a minimum of 3 months did not alter the pharmacokinetic profile of either methotrexate or 7-hydroxymethotrexate. Specifically, the peak plasma concentration and area under the plasma concentration-time curve of methotrexate and 7-hydroxymethotrexate were within the 0.80 to 1.25 boundaries. Methscopolamine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Methyclothiazide: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Methylphenidate: (Minor) The effects of gastrointestinal pH alterations on the absorption of extended-release methylphenidate (Ritalin LA) have not been studied. Per the manufacturer of extended-release methylphenidate, the modified release characteristics are pH-dependent. It is possible that the administration of proton pump inhibitors (PPIs) or other acid suppressants could alter the release of extended-release methylphenidate, resulting in reduced or increased absorption. Patients receiving a PPI should be monitored for adverse effects and reduced therapeutic efficacy of extended-release methylphenidate. Metolazone: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Mitotane: (Moderate) Use caution if mitotane and esomeprazole are used concomitantly, and monitor for decreased efficacy of esomeprazole and a possible change in dosage requirements. Mitotane is a strong CYP3A4 inducer and esomeprazole is a CYP3A4 substrate; coadministration may result in decreased plasma concentrations of esomeprazole. Modafinil: (Minor) Some manufacturers recommend avoiding the coadministration of hepatic cytochrome P-450 enzyme inducers and proton pump inhibitors (PPIs). Modafinil induces hepatic cytochrome P-450 enzyme CYP3A4 but significantly inhibits CYP2C19; both of these enzymes are responsible for the metabolism of PPIs. It is unclear that the theoretical interaction would result in a net increase or decrease in PPI action. If modafinil and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy, or for signs of PPI side effects. Mycophenolate: (Moderate) Concomitant administration of proton pump inhibitors (PPIs) with mycophenolate mofetil (Cellcept) appears to reduce MPA exposure AUC-12h (25.8 +/- 6.4 mg/L x h with omeprazole vs. 33.3 +/- 11.5 mg//L x h without omeprazole); however, the interaction does not appear to exist with mycophenolate sodium delayed-release tablets (Myfortic). Reduced systemic exposure of MPA after mycophenolate mofetil in the presence of a PPI appears to be due to impaired absorption of mycophenolate mofetil which may occur because of incomplete dissolution of mycophenolate mofetil in the stomach at elevated pH. The clinical significance of reduced MPA exposure is unknown; however patients should be evaluated periodically if mycophenolate mofetil is administered with a PPI. Of note, MPA concentrations appear to be reduced in the initial hours after mycophenolate mofetil receipt but increase later in the dosing interval because of enterohepatic recirculation. A second peak in the concentration-time profile of MPA is observed 612 hours after dosing due to enterohepatic recirculation. For example, the 12-hour plasma concentrations of MPA were similar among patients who received mycophenolate mofetil with or without omeprazole. The biphasic plasma concentration-time course of MPA due to extensive enterohepatic circulation hampers therapeutic drug monitoring of MPA. Drug exposure as measured by AUC-12h is the best estimator for the clinical effectiveness of mycophenolate, but measurement of full-dose interval MPA AUC-12h requires collection of multiple samples over a 12-hour period; MPA predose concentrations correlate poorly with MPA AUC-12h. The interaction does not appear to exist with Mycophenolate sodium (Myfortic). Nelfinavir: (Major) Use of proton pump inhibitors with nelfinavir is not recommended. Coadministration may result in decreased nelfinavir exposure, subtherapeutic antiretroviral activity, and possibility resistant HIV mutations. In one study, concurrent use of nelfinavir with omeprazole resulted in decreased nelfinavir AUC, Cmax, and Cmin by 36%, 37%, and 39%, respectively. Neratinib: (Major) Avoid concomitant use of neratinib with proton pump inhibitors due to decreased absorption and systemic exposure of neratinib; the solubility of neratinib decreases with increasing pH of the GI tract. Concomitant use with lansoprazole decreased neratinib exposure by 65%. Nilotinib: (Major) Avoid the concomitant use of nilotinib and proton pump inhibitors (PPIs), as PPIs may cause a reduction in nilotinib bioavailability. Nilotinib displays pH-dependent solubility with decreased solubility at a higher pH. PPIs inhibit gastric acid secretion and elevate the gastric pH. Administration of a single 400-mg nilotinib dose with multiple oral doses of esomeprazole 40 mg/day reduced the nilotinib AUC by 34% in a study in healthy subjects. Increasing the dose is unlikely to compensate for the loss of nilotinib exposure; additionally, separating the administration of these agents may not eliminate the interaction as PPIs affect the pH of the upper GI tract for an extended period of time. Octreotide: (Minor) The effectiveness of proton pump inhibitors may be decreased if given with other antisecretory agents, such as octreotide. Proton pump inhibitors inhibit only actively secreting H+-pumps. Antacids may be used while taking esomeprazole. Ombitasvir; Paritaprevir; Ritonavir: (Moderate) Concurrent administration of esomeprazole with ritonavir may result in elevated esomeprazole plasma concentrations. Esomeprazole is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Monitor patients for increased side effects if these drugs are administered together. Oritavancin: (Moderate) Coadministration of oritavancin and esomeprazole may result in increase in esomeprazole exposure. Esomeprazole is primarily metabolized by CYP2C19, but is also metabolized by CYP3A4. Oritavancin weakly induces CYP3A4, while weakly inhibiting CYP2C19. Coadministration of oritavancin and omeprazole resulted in a 15% increase in the ratio of omeprazole to 5-OH-omeprazole. If these drugs are administered concurrently, monitor the patient for signs of toxicity. Oxybutynin: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Pazopanib: (Major) Pazopanib displays pH-dependent solubility with decreased solubility at a higher pH. The concomitant use of pazopanib and proton pump inhibitors (PPIs) that elevate the gastric pH may reduce the bioavailability of pazopanib. In a study of patients with solid tumors, the AUC and Cmax of pazopanib were decreased by approximately 40% when coadministered with esomeprazole. If a drug is needed to raise the gastric pH, consider use of a short-acting antacid; separate antacid and pazopanib dosing by several hours. Pentobarbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Phenobarbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Phenytoin: (Moderate) Esomeprazole, which is an inhibitor of CYP2C19, may lead to increased levels of phenytoin, a substrate of CYP2C19. During clinical drug interaction studies, the changes in phenytoin concentrations appeared unlikely to be of clinical significance for most patients. However, it is advisable to monitor phenytoin levels and for hydantoin toxicity during concurrent treatment. Drugs known to induce CYP2C19 or CYP3A4 or both, such as phenytoin, may lead to decreased esomeprazole serum levels and patients should be monitored for expected clinical benefit during PPI treatment. Polyethylene Glycol; Electrolytes; Bisacodyl: (Minor) The concomitant use of bisacodyl oral tablets with drugs that raise gastric pH like proton pump inhibitors can cause the enteric coating of the bisacodyl tablets to dissolve prematurely, leading to possible gastric irritation or dyspepsia. When taking bisacodyl tablets, it is advisable to avoid PPIs within 1 hour before or after the bisacodyl dosage. Ponatinib: (Major) Ponatinib displays pH-dependent aqueous solubility; therefore, concomitant use of ponatinib and proton-pump inhibitors, such as esomeprazole, may result in decreased bioavailability and plasma exposure of ponatinib. Avoid concomitant use of ponatinib with proton-pump inhibitors unless the benefit outweighs the possible risk of ponatinib underexposure. If the use of both agents is necessary, monitor patients for signs of reduced efficacy. Posaconazole: (Major) The concurrent use of posaconazole oral suspension and proton pump inhibitors (PPIs) should be avoided, if possible, due to the potential for decreased posaconazole efficacy. If used in combination, closely monitor for breakthrough fungal infections. PPIs increase gastric pH, resulting in decreased posaconazole absorption and lower posaconazole plasma concentrations. When a single 400 mg dose of posaconazole oral suspension was administered with esomeprazole (40 mg PO daily), the mean reductions in Cmax were 46% and the mean reductions in AUC were 32% for posaconazole. The pharmacokinetics of posaconazole delayed-release tablets are not significantly affected by PPIs. Additionally, posaconazole is a potent inhibitor of CYP3A4, an isoenzyme partially responsible for the metabolism of many PPIs (dexlansoprazole, esomeprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole). Coadministration may result in increased plasma concentration of the PPIs. Primidone: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Propantheline: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Rifabutin: (Major) Some manufacturers recommend avoiding the coadministration of rifampin and proton pump inhibitors (PPIs). Rifamycins induce multiple hepatic cytochrome P-450 enzymes, including those responsible for the metabolism of PPIs. A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If rifampin and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. Rifampin: (Major) Some manufacturers recommend avoiding the coadministration of rifampin and proton pump inhibitors (PPIs). Rifamycins induce multiple hepatic cytochrome P-450 enzymes, including those responsible for the metabolism of PPIs. A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If rifampin and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. Rifamycins: (Major) Some manufacturers recommend avoiding the coadministration of rifampin and proton pump inhibitors (PPIs). Rifamycins induce multiple hepatic cytochrome P-450 enzymes, including those responsible for the metabolism of PPIs. A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If rifampin and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. Rifapentine: (Major) Some manufacturers recommend avoiding the coadministration of rifampin and proton pump inhibitors (PPIs). Rifamycins induce multiple hepatic cytochrome P-450 enzymes, including those responsible for the metabolism of PPIs. A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If rifampin and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. Rilpivirine: (Severe) Concurrent use of proton pump inhibitors and rilpivirine is contraindicated; when these drugs are coadministered, there is a potential for treatment failure and/or the development of rilpivirine or NNRTI resistance. Proton pump inhibitors inhibit secretion of gastric acid by proton pumps thereby increasing the gastric pH; for optimal absorption, rilpivirine requires an acidic environment. Coadministration of a proton pump inhibitor and rilpivirine may result in decreased rilpivirine absorption/serum concentrations, which could cause impaired virologic response to rilpivirine. Risedronate: (Major) Use of proton pump inhibitors (PPIs) with delayed-release risedronate tablets (Atelvia) is not recommended. Co-administration of drugs that raise stomach pH increases risedronate bioavailability due to faster release of the drug from the enteric coated tablet. This interaction does not apply to risedronate immediate-release tablets. In healthy subjects who received esomeprazole for 6 days, the Cmax and AUC of a single dose of risedronate delayed-release tablets (Atelvia) increased by 60% and 22%, respectively. PPIsare widely used and are frequently coadministered in users of oral bisphosphonates. A national register-based, open cohort study of 38,088 elderly patients suggests that those who use PPIs in conjunction with alendronate have a dose-dependent loss of protection against hip fracture. While causality was not investigated, the dose-response relationship noted during the study suggested that PPIs may reduce oral alendronate efficacy, perhaps through an effect on absorption or other mechanism, and therefore PPIs may not be optimal agents to control gastrointestinal complaints. Study results suggest that the interaction may occur across the class; however, other interactions have not been confirmed and data suggest that fracture protection is not diminished when risedronate is used with PPIs. A post hoc analysis of patients who took risedronate 5 mg daily during placebo-controlled clinical trials determined that risedronate significantly reduced the risk of new vertebral fractures compared to placebo, regardless of concomitant PPI use. PPI users (n = 240) and PPI non-users (n = 2489) experienced fracture risk reductions of 57% (p = 0.009) and 38% (p Ritonavir: (Moderate) Concurrent administration of esomeprazole with ritonavir may result in elevated esomeprazole plasma concentrations. Esomeprazole is metabolized by the hepatic isoenzyme CYP3A4; ritonavir is an inhibitor of this enzyme. Monitor patients for increased side effects if these drugs are administered together. Saquinavir: (Major) Coadministration with omeprazole results in significantly increased saquinavir concentrations. A similar interaction is expected with all proton pump inhibitors (PPIs). If saquinavir must be administered with PPIs, the patient should be closely monitored for saquinavir-related toxicities, including gastrointestinal symptoms, increased triglycerides, and deep vein thrombosis (DVT). Coadministration with omeprazole results in significantly increased saquinavir concentrations. In a small study, 18 healthy individuals received saquinavir 1000 mg (with ritonavir 100 mg) twice daily for 15 days; on days 11 through 15 omeprazole 40 mg was given once daily, which resulted in an 82% increase in the saquinavir AUC. A similar interaction is expected with all PPIs. Scopolamine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Secobarbital: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Secretin: (Major) Discontinue use of proton pump inhibitors before administering secretin. Patients who are receiving proton pump inhibitors at the time of stimulation testing may be hyperresponsive to secretin stimulation, falsely suggesting gastrinoma. The time required for serum gastrin concentrations to return to baseline after discontinuation of a proton pump inhibitor is specific to the individual drug. Sertraline: (Moderate) In one study using a small number of subjects taking sertraline relative to the other SSRIs studied, sertraline concentrations were increased by approximately 38.5% during coadministration with esomeprazole, a CYP2C19 inhibitor. However, the clinical significance of the interaction is not proven, as sertraline is metabolized by multiple CYP enzymes, not just CYP2C19, and inhibition by one pathway does not usually influence sertraline pharmacokinetics. Sofosbuvir; Velpatasvir: (Major) Coadministration of proton pump inhibitors (PPIs) with velpatasvir is not recommended. If it is considered medically necessary to coadminister, velpatasvir should be administered with food and taken 4 hours before omeprazole 20 mg. Other PPIs have not been studied; however, it may be prudent to separate the administration of the other PPIs similarly. Velpatasvir solubility decreases as pH increases; therefore, drugs that increase gastric pH are expected to decrease the concentrations of velpatasvir, potentially resulting in loss of antiviral efficacy. Sofosbuvir; Velpatasvir; Voxilaprevir: (Major) Coadministration of proton pump inhibitors (PPIs) with velpatasvir is not recommended. If it is considered medically necessary to coadminister, velpatasvir should be administered with food and taken 4 hours before omeprazole 20 mg. Other PPIs have not been studied; however, it may be prudent to separate the administration of the other PPIs similarly. Velpatasvir solubility decreases as pH increases; therefore, drugs that increase gastric pH are expected to decrease the concentrations of velpatasvir, potentially resulting in loss of antiviral efficacy. Solifenacin: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. St. John’s Wort, Hypericum perforatum: (Major) Coadministration of St. John’s Wort, Hypericum perforatum (300 mg three times daily) for 14 days with a one time dose of omeprazole (20 mg) on day 15 resulted in decreased omeprazole plasma concentrations in healthy subjects. Omeprazole AUC was reduced by approximately 40% in both poor and extensive metabolizers of CYP2C19. The clinical significance of this interaction is not clear; however, due to variations in the amounts of active ingredient in herbal products, the magnitude of this interaction and the resultant clinical effect may vary. St. John’s Wort induces both CYP3A4 and CYP2C19 dependent metabolism of omeprazole. Since, proton pump inhibitors (PPIs) are primary substrates of the CYP2C19 enzyme, patients taking St. John’s Wort concomitantly with a PPI should be monitored for PPI efficacy. Sucralfate: (Minor) Sucralfate may delay absorption and reduce the bioavailability of lansoprazole. Lansoprazole should be taken no less than 30 minutes before sucralfate. This interaction is theoretical and is based on the interaction between sucralfate and lansoprazole; sucralfate has been shown to delay absorption and reduce the bioavailability of lansoprazole by about 17%. No information is available to determine if a similar interaction occurs with esomeprazole. Tacrolimus: (Moderate) Esomeprazole may increase tacrolimus whole blood trough concentrations and increase the risk of serious adverse reactions (e.g., neurotoxicity, nephrotoxicity, QT prolongation). Monitor tacrolimus whole blood trough concentrations and reduce the tacrolimus dose if needed. Tacrolimus is metabolized primarily by CYP3A4; esomeprazole inhibits CYP3A4 and thus may decrease CYP3A4-mediated metabolism of tacrolimus. Telaprevir: (Moderate) Coadministration may result in elevated esomeprazole plasma concentrations. Although clinical trials found no doses adjustments are needed for either medication, close monitoring is advised when administering esomeprazole with telaprevir due to the potential for esomeprazole-related adverse events. Esomeprazole is partially metabolized by the hepatic isoenzyme CYP3A4; telaprevir inhibits this isoenzyme. Telithromycin: (Minor) Concentrations of esomeprazole may be increased with concomitant use of telithromycin. Esomeprazole is a CYP3A4 substrate and telithromycin is a strong CYP3A4 inhibitor. Patients should be monitored for increased side effects. Telotristat Ethyl: (Moderate) Use caution if coadministration of telotristat ethyl and esomeprazole is necessary, as the systemic exposure of esomeprazole may be decreased resulting in reduced efficacy. If these drugs are used together, monitor patients for suboptimal efficacy of esomeprazole; consider increasing the dose of esomeprazole if necessary. Esomeprazole is a CYP3A4 substrate. The mean Cmax and AUC of another sensitive CYP3A4 substrate was decreased by 25% and 48%, respectively, when coadministered with telotristat ethyl; the mechanism of this interaction appears to be that telotristat ethyl increases the glucuronidation of the CYP3A4 substrate. Thiazide diuretics: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with thiazide diuretics (chlorothiazide, hydrochlorothiazide, indapamide, and metolazone). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Thiopental: (Major) Avoid coadministration of esomeprazole with barbiturates because it can result in decreased efficacy of esomeprazole. Esomeprazole is extensively metabolized in the liver by CYP2C19 and CYP3A4. Barbiturates induce CYP3A4 and CYP2C19. Thyroid hormones: (Moderate) The use of proton pump inhibitors may result in decreased effectiveness of thyroid hormone therapy. Monitor clinically for signs and symptoms of hypothyroidism and altered response to thyroid hormone therapy. Periodically assess the TSH during use of these drugs together. Gastric acidity is an essential requirement for proper and adequate absorption of levothyroxine and other thyroid hormones. Proton pump inhibitors may cause hypochlorhydria, affect intragastric pH, and reduce thyroid hormone absorption. Ticlopidine: (Minor) Ticlopidine may inhibit the CYP2C19 isoenzyme, leading to increased plasma levels of drugs that are substrates for the CYP2C19 isoenzyme, such as esomeprazole. Tipranavir: (Moderate) Some manufacturers recommend avoiding the coadministration of hepatic cytochrome P-450 enzyme inducers and proton pump inhibitors (PPIs). Tipranavir markedly induces the hepatic cytochrome P-450 enzyme CYP2C19, an enzyme responsible for the metabolism of PPIs. However, since tipranavir is not given unless it is co-prescribed with ritonavir, a known marked enzyme inhibitor, a reduction in PPI metabolism may be unlikely to occur. A reduction in PPI concentrations may increase the risk of gastrointestinal (GI) adverse events such as GI bleeding. If tipranavir and PPIs must be used together, monitor the patient closely for signs and symptoms of GI bleeding or other signs and symptoms of reduced PPI efficacy. Tolterodine: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Torsemide: (Moderate) Proton pump inhibitors, such as esomeprazole, have been associated with hypomagnesemia. Hypomagnesemia occurs with loop diuretics (furosemide, bumetanide, torsemide, and ethacrynic acid). Low serum magnesium may lead to serious adverse events such as muscle spasm, seizures, and arrhythmias. Therefore, clinicians should monitor serum magnesium concentrations periodically in patients taking a PPI and diuretics concomitantly. Patients who develop hypomagnesemia may require PPI discontinuation in addition to magnesium replacement. Trihexyphenidyl: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Trospium: (Moderate) The American College of Gastroenterology states that the effectiveness of proton pump inhibitors (PPIs) may be theoretically decreased if given with other antisecretory agents (e.g., anticholinergics). Proton pump inhibitors (PPIs) inhibit only actively secreting H+-pumps. Vemurafenib: (Moderate) Coadministration of vemurafenib and esomeprazole could lead to decreased esomeprazole concentrations and efficacy. Vemurafenib is a CYP3A4 inducer and esomeprazole is a CYP3A4 substrate. Monitor patients for efficacy. Voriconazole: (Moderate) Monitor for increased drug toxicity as coadministration of esomeprazole and voriconazole may result in increased concentrations of both drugs. Although dose adjustments are not generally needed, patients with Zollinger-Ellison’s syndrome who often require higher esomeprazole doses (up to 240mg/day) may require an adjustment in esomeprazole dose. Esomeprazole is metabolized primarily by CYP2C19 and secondarily by CYP3A4 and is also a CYP2C19 inhibitor; voriconazole is a CYP2C19 substrate and inhibitor of CYP2C19 and CYP3A4. Warfarin: (Moderate) Omeprazole (CYP2C19 inhibitor) can prolong the elimination of warfarin, particularly R-warfarin which is partially metabolized by CYP2C19. The combined use of omeprazole and warfarin has been associated with reports of increased INR and prothrombin time (PT). In addition, post-marketing reports of the combination of esomeprazole and warfarin have indicated elevations in PT. There have been reports of increased International Normalized Ratio (INR) and prothrombin time in patients receiving other proton pump inhibitors (PPIs) (including esomeprazole, lansoprazole, rabeprazole, and pantoprazole and warfarin concomitantly. It is prudent to monitor the INR more closely if these agents are combined with warfarin.
There are no adequate and well-controlled studies regarding use of esomeprazole during human pregnancy. Esomeprazole is the S-isomer of omeprazole. Current data, including epidemiologic data and an expert review by TERIS (the Teratogen Information System), fail to demonstrate an increased risk of major congenital malformations or other adverse pregnancy outcomes with first trimester omeprazole use. Animal reproductive studies have been conducted with omeprazole and esomeprazole. Rats and rabbits dosed with omeprazole experienced dose-dependent embryo-lethality at omeprazole doses that were approximately 3.4 to 34 times an oral human dose of 40 mg, based on a body surface area (BSA) for a 60 kg person. Teratogenicity was not observed in animal reproduction studies with administration of oral esomeprazole in rats and rabbits during organogenesis with doses about 68 and 42 times, respectively, an oral human dose of 40 mg esomeprazole or 40 mg omeprazole, based on BSA for a 60 kg person. However, changes in bone morphology were observed in offspring of rats dosed through most of pregnancy and lactation at doses greater than or equal to 33.6 times an oral human dose of 40 mg. Although animal studies are not always predictive of human effects, because of the observed effect at high doses of esomeprazole magnesium on developing bone in rat studies, esomeprazole use in pregnancy should be limited. Esomeprazole, like omeprazole, is expected to cross the human placenta. Epidemiological evaluations have compared the rate of congenital abnormalities and stillbirths among those exposed to omeprazole in utero during pregnancy to similar findings for those exposed to H2-receptor antagonists or other controls. Overall, slightly higher rates of congenital malformations (e.g., ventricular septal defects) and number of stillborns have been reported for cases where exposure to omeprazole occurred in the first trimester of pregnancy and beyond. Use during pregnancy should be limited to cases where the benefit to the mother outweighs any potential risk to the fetus. In 2009, a population-based observational cohort study explored a possible link between gastric acid suppressive therapy (e.g., proton pump inhibitors) during pregnancy and a diagnosis of allergic disease or a prescription for asthma or allergy medications in the exposed child. Among the cohort (n = 585,716), 1% of children exposed to gastric acid suppressive drugs in pregnancy received a diagnosis of allergic disease. For developing allergy or asthma, an increased OR of 1.43 and 1.51, respectively, were observed regardless of drug used, time of exposure during pregnancy, and maternal history of disease. Proposed possible mechanisms for a link include: (1) exposure to increased amounts of allergens could cause sensitization to digestion-labile antigens in the fetus; (2) the maternal Th2 cytokine pattern could promote an allergy prone phenotype in the fetus; (3) maternal allergen specific immunoglobulin could cross the placenta and sensitize fetal immune cells to food and airborne allergens. Study limitations were present and confirmation of results is necessary before further conclusions can be drawn from this data. Risk versus benefit should be considered prior to use. Self-medication with esomeprazole (OTC formulations) during pregnancy is not recommended. Esomeprazole strontium use during pregnancy should only be considered if the potential benefit justifies the potential risk to the fetus. Strontium is known to compete with calcium for intestinal absorption and is incorporated into bone. Because of the effect of esomeprazole strontium observed at high doses on developing bone in animal studies, its use in pediatric patients is not recommended; thus, passage of strontium to a developing fetus is not advisable; alternate therapies should be considered. Pregnant patients should see their health care professional for a proper diagnosis and for treatment recommendations.
Esomeprazole strontium use during breast-feeding should be avoided. Strontium is known to compete with calcium for intestinal absorption and is incorporated into bone. Because of the effect of esomeprazole strontium observed at high doses on developing bone in animal studies, its use in pediatric patients is not recommended; passage to a nursing infant through breast milk should also be avoided. There are no clinical data on the effects of esomeprazole on the nursing infant or on milk production. The developmental and health benefits of breast-feeding should be considered along with the mother’s clinical need for esomeprazole and any potential adverse effects on the nursing infant from esomeprazole or from the underlying maternal condition.Esomeprazole has a low molecular weight (345) and excretion into breast milk is expected. Esomeprazole is the S-isomer of omeprazole and limited data suggest that omeprazole may be present in human milk. One study reported the use of omeprazole in late gestation and continued use through lactation. During breast-feeding, the mother fed her infant prior to a dose of 20 mg of omeprazole. Samples of expressed milk were analyzed and a maximum daily exposure to the infant was calculated to be 4 mcg (based on the consumption of 200 mL of milk/day). Based on the above case, a maximum dose of 3 mcg/kg daily or about 0.9% of the maternal weight-adjusted dosage would be delivered to an exclusively breast-fed infant based on a milk consumption of 150 mL/kg/day. For comparison, doses of 0.5 mg/kg PO once daily for 6 weeks have been studied during infancy (age 2.9 +/- 0.9 months) for peptic esophagitis. Nevertheless, the methods of collection and calculations of the sampled milk were not clearly defined in this case report. Milk expressed early in feeding contains less lipid content as compared to milk expressed towards the end of feeding. Taking into account that omeprazole is a lipid soluble drug, milk expressed and analyzed early on in feeding may not accurately reveal the true exposure to a feeding infant. Potentially serious adverse reactions may occur with the use of omeprazole or esomeprazole during breast-feeding, including suppression of gastric acid secretion in the nursing infant. Alternative therapies for consideration include antacids and H2 blockers. Some experts recommend that consideration of the dose and drug properties may allow for continued nursing without significant exposure to the breast-fed infant for nursing women who require esomeprazole. If possible, the mother should wait to nurse or express milk 5 to 7.5 hours after the daily dose of esomeprazole. Allowing this time should eliminate 97% of the drug from the plasma and would avoid the period when the greatest amount of drug is available to enter the milk. Near the end of the waiting period, breast milk should be expressed and discarded to complete the strategy to limit the infant’s exposure to esomeprazole. This strategy is based on known pharmacokinetic parameters such as half-life; however, further study is warranted examining the use of this strategy in human mother-infant pairs.
Esomeprazole is a substituted benzimidazole proton-pump inhibitor (PPI) that suppresses gastric acid secretion by inhibiting the gastric (H+, K+)-ATPase enzyme pump. Following activation in an acidic pH, esomeprazole binds irreversibly to the H+/K+ ATPase pump on the secretory surface of the parietal cell membrane. Subsequently, the secretion of hydrogen ions into the gastric lumen is inhibited. Gastric acid pump inhibitors block the final step of gastric acid production, and inhibit both basal and stimulus-induced acid secretion. Delayed-release doses of 20 mg and 40 mg esomeprazole maintained intragastric pH > 4.0 for 12.7 hours and 16.8 hours, respectively. Significant in vitro activity against Helicobacter pylori (H. Pylori) has been demonstrated for esomeprazole. Esomeprazole monotherapy increases the clearance rate of H. pylori; however, eradication does not occur without appropriate antimicrobial therapy. Similar to omeprazole and other PPIs, hypergastrinemia can occur during esomeprazole therapy. Although prolonged hypergastrinemia has been associated with gastric tumors in rats, long-term studies of proton pump inhibitors do not suggest the development of tumors in humans.
Esomeprazole is administered orally and intravenously. It is 97% bound to plasma proteins. Metabolism occurs extensively in the liver to inactive metabolites via CYP2C19 and to a lesser extent by CYP3A4. The metabolites lack antisecretory activity. The plasma elimination half-life is approximately 1.5 hours. Less than 1% of parent drug is excreted in the urine with the remainder excreted as inactive metabolites in both the urine and feces. Affected cytochrome P450 enzymes: CYP2C19, CYP3A4Esomeprazole is metabolized by CYP2C19 and CYP3A4, and it inhibits the CYP2C19 isoenzyme. In vitro and in vivo drug interaction studies note that it is not likely to inhibit CYP3A4, CYP1A2, CYP2A6, CYP2C9, CYP2D6, or CYP2E1.
Esomeprazole dissolves rapidly in an acidic environment and therefore is formulated as a capsule containing enteric-coated pellets. Multiple dosing at 40 mg/day results in 90% bioavailability versus 64% after a single 40 mg dose. Cmax is reached within 1—3.5 hours. The AUC of esomeprazole (the S-isomer) is 80% higher than with omeprazole (both S- and R-isomer) due to decreased clearance and first-pass elimination of the S-isomer. Clinically this allows more esomeprazole to reach the site of action and may contribute to higher efficacy rates. The AUC of a single 40 mg dose of esomeprazole is decreased by 33—53% after food intake compared to fasting conditions.
The pharmacokinetics of intravenous esomeprazole were determined in healthy adult subjects following once daily administration of 20 mg and 40 mg by constant rate of infusion over 30 minutes for 5 days. The pharmacokinetic profile for the 20 mg and 40 mg dose is as follows: AUC (5.11 and 16.21 micromoles x h/L, respectively) and Cmax (3.86 and 7.51 micromoles/L, respectively).
US-based MDs, DOs, NPs and PAs in full-time patient practice can register for free on PDR.net. PDR.net is to be used only as a reference aid. It is not intended to be a substitute for the exercise of professional judgment. You should confirm the information on the PDR.net site through independent sources and seek other professional guidance in all treatment and diagnosis decisions.
© document.write(new Date().getFullYear()) PDR, LLC. All rights reserved.